Many women face headaches that seem to appear out of nowhere, often around the same time each month. These are known as hormonal headaches, and they are closely tied to changes in the body’s hormone levels. Hormonal fluctuations, especially drops in estrogen, are a key reason why headaches and migraines are much more common in women than in men, particularly around menstruation Headaches and hormones connection.

Hormonal headaches may show up during menstruation, pregnancy, or even menopause, and can cause pain, tiredness, and sensitivity to light or sound. Symptoms range from mild aches to severe migraines, and some women may also feel more tired than usual when these headaches strike menstrual migraines and symptoms. Learning how hormones affect headache risk is the first step toward managing or even preventing these painful attacks.
Key Takeaways
- Hormonal changes often trigger headaches for many women.
- Symptoms can include pain, tiredness, and light sensitivity.
- Management involves lifestyle changes, treatment, or talking with a doctor.
What Are Hormonal Headaches?
Hormonal headaches are linked to changes in hormone levels, especially in women. Fluctuations in estrogen and progesterone can trigger different types of headaches at various stages of life.
Defining Hormonal Headaches
Hormonal headaches are types of headaches that are directly connected with changes in hormone levels. These headaches often occur in women around their menstrual periods, pregnancy, or menopause.
Most hormonal headaches are migraine-type. Instead of dull, mild pain, they often produce intense, throbbing pain usually on one side of the head. People may also experience sensitivity to light, nausea, or vision changes during a hormonal headache.
Hormonal headaches tend to have predictable timing, such as just before a woman’s menstrual period. The main difference from other headaches is the clear link to hormone changes in the body.
How Hormones Influence Headaches
Hormones, like estrogen and progesterone, are chemicals that control many functions in the body. When these hormones fluctuate, they can affect the brain’s chemistry and blood vessels, which can trigger headaches.
A drop in estrogen, especially before a woman’s period, is a common cause for migraines and is discussed further by the Mayo Clinic. These changes can make the nerve cells in the brain more sensitive to pain signals.
Other times in life with big hormone changes, like during pregnancy or menopause, can also lead to headaches. Some women get fewer headaches when their hormones are steady during pregnancy, while others experience more around menopause.
Prevalence Among Women
Hormonal headaches occur much more often in women than in men. This difference is mostly because women’s hormone levels change more throughout their lives for reasons like periods, pregnancy, and menopause.
About 60% to 70% of women who get migraines notice a link between their headaches and their menstrual cycle, as reported by Johns Hopkins Medicine. These headaches can start at puberty and may decrease after menopause.
Not all women will experience hormonal headaches the same way. Some may get them only around their periods, while others notice headaches during other times when estrogen levels change.
Hormonal Triggers for Headaches
Certain hormone changes in a woman’s body often play a major role in the development of headaches. Fluctuations in estrogen and progesterone, as well as the timing of these changes, have specific effects on headache patterns and severity.
Menstrual Cycle Fluctuations
Headaches often worsen during the menstrual cycle due to hormonal changes. Many women notice they get migraines or tension headaches right before or during their period. This pattern is linked to the drop in estrogen that happens at the end of the cycle.
People can track this pattern by noting when headaches occur each month. Keeping a headache diary may help to identify hormonal triggers and predict when headaches are likely. Timing and severity may differ from person to person.
According to clinics and experts, migraines triggered by menstruation are called menstrual migraines. These headaches can be more difficult to treat, sometimes lasting longer than non-menstrual migraines. Some women have headaches only around their period, while others experience them at other times too.
Understanding the connection between the menstrual cycle and headaches can help in managing them better.
Estrogen Withdrawal and Headache Onset
A rapid drop in estrogen, called estrogen withdrawal, is a common cause for hormonal headaches. This sudden change most often occurs just before menstruation. Estrogen is thought to protect against headaches, so when levels fall sharply, the risk of migraines goes up.
Estrogen withdrawal can also happen at other times, such as after stopping hormonal birth control or during menopause. Each time estrogen levels drop quickly, some women may notice stronger or more frequent headaches.
Some treatment options focus on stabilizing estrogen or delaying its withdrawal to lower the risk of headaches. For example, certain types of hormonal therapy or consistent use of birth control pills may help some women. More about how estrogen withdrawal triggers headaches is available from health resources.
Role of Progesterone
While estrogen often gets the most attention, progesterone also plays a part in hormone-related headaches. Progesterone levels rise after ovulation and fall just before the period starts, along with estrogen. Changes in progesterone may add to or trigger headaches in some women, though the link is not as strong as with estrogen.
Some women notice headaches get worse in the second half of their cycle. This is when progesterone is higher. A drop in both estrogen and progesterone together before a period may make headaches more severe or longer-lasting.
Research is still looking into how progesterone may affect migraines or tension headaches. Treatment often focuses on estrogen, but in some cases, adjusting both hormone levels could help.
Other Hormone Variations
Other hormonal changes may also play a role in headache patterns. Pregnancy, perimenopause, and menopause all come with major hormone shifts. For example, during pregnancy, estrogen remains high and steady, which often leads to fewer headaches for some women.
After childbirth, estrogen levels drop quickly, and headaches may return. The start of menopause means more frequent hormone changes, which can also trigger headaches or migraines. Hormone replacement therapy (HRT) can sometimes cause more headaches or make them worse, especially if estrogen doses are not consistent or if the body is sensitive to these changes.
Understanding how different hormone variations affect headaches can help women and their healthcare providers plan the best way to reduce or prevent these symptoms.
Types of Women’s Hormonal Headaches
Hormonal headaches in women are often tied to changes in estrogen levels. Migraine headache patterns, timing, and triggers may differ depending on the phase of the menstrual cycle and the type of migraine.
Menstrual Migraines
Menstrual migraines are a specific type of migraine that occur around the time of a woman's period. These migraines are closely linked to the natural drop in estrogen that happens just before menstruation. This decrease in hormones often makes women more likely to experience a migraine attack two days before their period starts and up to three days after it begins.
Symptoms tend to include throbbing head pain, nausea, and sensitivity to light. These migraines are usually more severe than other types of headaches. Treatments may involve both medicine used for regular migraines and sometimes preventative medications taken before a woman's period. Learn more about how hormonal changes like estrogen drops can cause menstrual migraines.
Menstrually Related Migraine
Menstrually related migraine (MRM) describes migraines that are linked to the menstrual cycle, but also occur at other times of the month. In this case, women may notice migraine attacks both around their period and during other weeks. The main trigger is still hormone changes, especially falling estrogen, but other factors like stress or certain foods may also play a role.
MRM can make it hard to predict when a migraine will happen. The headaches may be similar in intensity to menstrual migraines, including pain, light sensitivity, and possible nausea. Treatment often focuses on both stopping pain and trying to prevent frequent occurrences.
Pure Menstrual Migraine
Pure menstrual migraine is less common than other types. It refers to migraine attacks that happen only during the period and not at any other time during the cycle. These migraines are always timed with menstruation and are not triggered by other causes. The key factor for diagnosis is the consistent pattern tied strictly to the menstrual period.
Women experiencing pure menstrual migraine will notice that headaches start within the two days before their period or in the first three days of bleeding, but they do not have migraine attacks at any other time. Management may include tracking the menstrual cycle and using short-term preventive medicine before the expected onset. Further information on this type can be found in medical resources on menstrual migraines.
Life Stages and Hormonal Headache Risk
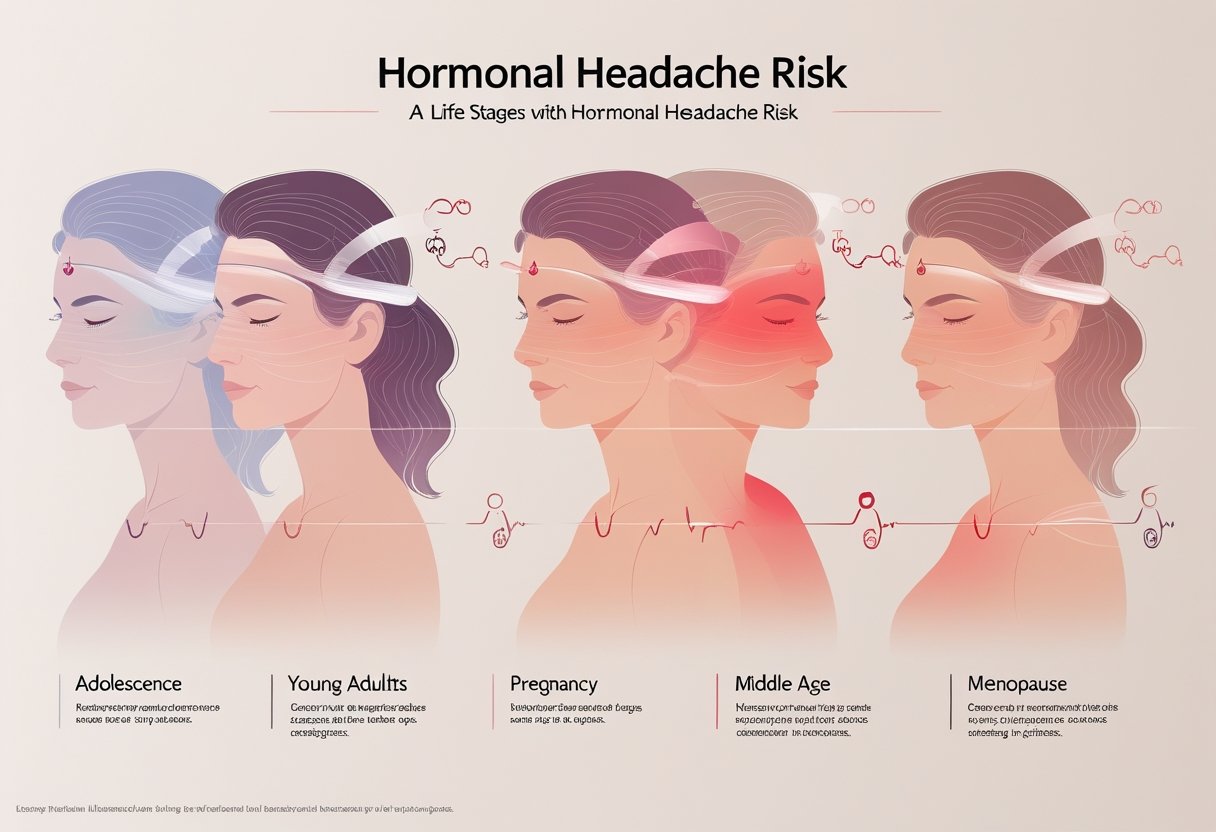
Hormonal headaches often begin with puberty, may worsen or improve during pregnancy, and change again as women approach menopause. Fluctuations in estrogen at each stage play a key role in when and how headaches develop.
Puberty and Adolescence
When girls reach puberty, major shifts in hormone levels occur. These hormonal changes can lead to a higher risk of headaches and migraines compared to boys the same age. Menstrual cycles usually start around this time, causing monthly ups and downs in estrogen.
Estrogen increases pain sensitivity, which is why some girls get headaches right before or during their periods. About half of young women with migraines notice a connection between headache frequency and their cycles. Keeping a headache diary can help track patterns and triggers.
Frequent headaches during adolescence may impact school activities and social life. Treatments may include over-the-counter pain medicines or seeing a doctor for more severe cases. Learning about hormonal triggers is key for managing symptoms at this stage, as monthly fluctuations are common and expected. For more details, see how hormones make headaches more likely.
Pregnancy-Related Headaches
During pregnancy, hormone levels change quickly, and many women notice differences in headache patterns. For some, migraines get better or even stop, while others may see no change or slight worsening.
Estrogen levels rise steadily throughout pregnancy, often leading to fewer headaches in the second and third trimesters. The first trimester, however, can still bring headaches or migraines because hormone levels shift rapidly at the start. Dehydration, stress, and poor sleep can make headaches worse during this time.
After birth, hormones drop sharply, which can trigger headaches or migraines, especially if a woman had them before pregnancy. Women should talk with their doctor about safe treatment options, since not all headache medicines are safe in pregnancy. For more information, see how life stages affect migraine in women.
Perimenopause and Menopause
As women enter perimenopause, hormone levels start to fluctuate more wildly. This phase can last for years and happens before menopause is complete. Many women notice an increase in headaches or migraines due to changing estrogen levels.
The start and end of menstrual cycles become unpredictable during perimenopause. Some women may have longer cycles or skipped periods. Migraine headaches often peak during this stage, but may improve after menopause when hormones finally stabilize.
During menopause, menstrual cycles stop and estrogen levels fall and stay low. This change can bring relief for many women, though some still get headaches. For those using hormone therapy, headaches may continue or shift due to ongoing hormone changes. To learn more, see how menopause and hormone therapy affect headaches.
Common Symptoms and Co-Occurring Issues

Hormonal headaches in women can cause more than just pain. They often appear with a mix of physical and sensory symptoms that make daily life more difficult.
Headache Pain Patterns
The headache pain that comes with hormonal changes is usually moderate to severe. Many women feel a throbbing or pulsing pain most often on one side of the head, though it can also affect both sides.
These headaches can last anywhere from a few hours to several days. The pain often gets worse with regular movement such as walking up stairs or bending down.
Migraine symptoms linked to hormones often peak just before or during the menstrual period. In many cases, these headaches are called menstrual migraines and can greatly impact daily routines.
Some women also report increased tenderness in the scalp, neck, or shoulders during these headaches.
Nausea and Vomiting
Nausea is a common issue that happens alongside hormonal migraines. Many women report feeling sick to their stomach, and some even vomit, especially when the pain is intense.
The risk of vomiting appears higher during stronger headaches. Nausea often makes it difficult to eat or drink, which can lead to more weakness or dehydration.
These symptoms tend to be worse when headaches are severe. The uneasy stomach feeling might come before, during, or after the peak of head pain. For some women, these issues may last even after the headache fades away.
Nausea and vomiting are especially linked to hormonal headaches and migraines, making this combination very challenging.
Fatigue and Sensory Sensitivities
Fatigue is another frequent problem. Many women feel tired or worn out before, during, or after a hormonal migraine. This tiredness can linger for a day or more, even after the main headache is gone.
Hormonal migraines often cause sensitivity to light, sound, or even smells. Bright lights, loud noises, or strong odors can quickly make the pain feel worse.
Some people need to rest in a quiet, dark room to find relief. Sensory triggers and fatigue together can make regular activities hard to manage.
Women with hormonal headaches are more likely to miss work or social events because of these symptoms, as noted by health sources like the Mayo Clinic.
Diagnosis and When to See a Specialist
Understanding the cause of hormonal headaches is important for managing them. Careful tracking and the help of a specialist can make a big difference in finding relief and building a treatment plan.
Symptom Tracking and Diagnosis
Women who notice headache patterns linked to their menstrual cycle or hormone changes should keep a headache diary. This diary should include the time, date, severity, and type of headache. It's important to note other symptoms like nausea, light sensitivity, and tiredness. Tracking hormone events, such as the start of the period, birth control use, or menopause symptoms, gives helpful clues.
Doctors may also ask about family history of migraine headaches. They might order blood tests or imaging if symptoms are severe or do not follow a clear pattern. A clear, detailed record helps health care providers choose the best treatment and rule out other causes, such as sinus issues or tension headaches.
Role of a Headache Specialist
A headache specialist is a doctor with extra training in treating complex and recurring headaches. If hormonal headaches are disabling or don't improve with basic treatments, it may be time to seek help from a specialist. They use advanced tools and knowledge to diagnose types of headaches.
Specialists may recommend prescription medicines, hormone therapy, or lifestyle changes based on the person’s needs. For cases linked to hormone swings, such as changes in estrogen and progesterone, a specialist can identify triggers and suggest targeted care strategies. Seeing a specialist ensures accurate diagnosis and helps prevent headaches from getting worse or becoming chronic.
Treatment Options for Hormonal Headaches
Hormonal headaches can be managed with different treatment strategies. Both prescription and non-prescription methods may help reduce pain, prevent attacks, or make symptoms easier to tolerate.
Acute Treatment Strategies
Pain relief medications are usually the first step for women dealing with hormonal headaches. Over-the-counter medicines such as acetaminophen, ibuprofen, and naproxen can reduce headache pain if taken early. Some women may benefit from specific NSAIDs like mefenamic acid or fenoprofen during the days before and during their period.
Prescription medicines called triptans (for example, sumatriptan) are very effective for stopping migraines once symptoms start. Triptans can be taken as pills, nasal sprays, or injections. Sometimes, doctors recommend ergotamines if other treatments do not work well enough.
Antiemetics (such as prochlorperazine or metoclopramide) are used if nausea or vomiting is a problem. They may be used alone or together with pain relievers to make treatment even more effective.
Preventive and Prophylactic Medications
Women with frequent or severe hormonal headaches may need medicines to stop attacks before they start. Nonsteroidal anti-inflammatory drugs (NSAIDs), like naproxen or ibuprofen, can be used a few days before the period starts and continued for several days.
Hormone therapies, such as estrogen pills, gels, or patches, can help prevent strong drops in estrogen that often trigger headaches. Birth control methods with stable estrogen levels, like the pill or vaginal ring, may lower the number of headaches some women have. Details about how these choices help can be found with estrogen supplementation or birth control for menstrual migraine.
For those with frequent migraines, doctors may also suggest other prophylactic medications. These could include certain blood pressure medicines, antidepressants, or anticonvulsants.
Non-Pharmacological Approaches
Lifestyle changes can help reduce hormonal headaches for some women. Keeping a regular sleep schedule, staying hydrated, and avoiding skipped meals are basic but important steps.
Stress management techniques like yoga, deep breathing, or relaxation therapy can lower tension and make headaches less likely. Tracking headache patterns in a diary helps many women pinpoint triggers and find better ways to cope.
Some women find relief with non-drug approaches like cold packs, rest in a dark room, or gentle neck massages. These practices may ease pain when used at the first sign of a headache. Combining these habits with medications might offer the best control.
Hormonal Therapies and Birth Control
Hormonal treatments impact headaches in different ways, depending on the medicine and the person’s hormonal balance. Some therapies can make headaches worse, while others may help reduce their frequency or intensity.
Oral Contraceptives and Headache Risk
Oral contraceptives, including birth control pills, can affect headache patterns in women. These pills often contain estrogen and progestin. Changes in hormone levels, especially drops in estrogen during the pill-free week, are a known trigger for headaches, including migraines.
Some women find that their headaches improve after starting oral contraceptives. For others, especially those with migraines with aura, these medications can make headaches worse. The risk of stroke is higher in women who have migraines with aura and use combination birth control pills. It is important for healthcare providers to consider a patient’s headache history before recommending these options.
For some women, using pills with a lower estrogen dose or taking them continuously may help reduce headache frequency. Individual response to birth control can vary, so regular follow-up and reevaluation are key. More details can be found in guidance from expert groups like the American Headache Society and recent research about birth control and headaches.
Hormone Replacement Therapy in Menopause
Hormone replacement therapy (HRT) is often used during menopause to help with symptoms such as hot flashes. It can also have effects on headaches. Fluctuating estrogen levels, which may happen at the start and end of HRT, can cause headaches or migraines in some women.
Estrogen patches and gels seem to cause fewer swings in hormone levels compared to pills, which may lower the chance of triggering headaches. Some women notice that headaches improve after starting HRT, while others may find that migraines become worse or more frequent.
Close monitoring is needed when starting or changing HRT. Adjusting the type, dose, or delivery method can make a difference. More information can be found through detailed medical resources like the Cleveland Clinic’s guide on hormone headaches.
Role of Tamoxifen
Tamoxifen is a medication often used in breast cancer treatment. It blocks the effects of estrogen on breast cells. While it is not usually used to treat headaches, it can change how headaches behave for some women by altering estrogen activity.
Tamoxifen may cause changes in migraine patterns or lead to new headaches, especially as the body adjusts to new hormone balances. These effects can be temporary or ongoing, depending on how a woman responds to the drug.
Anyone experiencing new or noticeably different headaches while taking tamoxifen should tell their healthcare provider. Monitoring and adjusting treatment may be needed if headaches become severe. The impact of tamoxifen on headaches depends on the individual’s sensitivity to hormones and the presence of other risk factors.
Lifestyle Factors and Headache Management
Managing hormonal headaches in women often requires changes in daily routines, healthy coping strategies for stress, and close attention to nutrition. Many women find relief by making small but important adjustments at home or with their diet.
Stress Management Techniques
High stress levels can trigger or worsen hormonal headaches. Stress can cause physical changes in the body, such as muscle tension and hormone shifts, that make headaches more likely.
Some useful techniques for stress management include deep breathing, meditation, yoga, and journaling. Regular physical activity, such as brisk walking or swimming, also helps lower stress and may prevent some headache episodes. Setting aside time each day for relaxation or hobbies can provide a good mental break. Many women benefit from setting a consistent sleep schedule, as lack of sleep or changes in sleep patterns can trigger headaches.
Notably, some women track their “headache triggers” in a journal, which can help them better understand and avoid stressful situations that often lead to symptoms.
Dietary and Lifestyle Modifications
Certain foods and habits influence headache patterns. Skipping meals or not drinking enough water may increase the chance of a headache. Eating regular, balanced meals and staying hydrated is important. Some women are sensitive to foods such as aged cheese, processed meats, chocolate, or high-caffeine drinks, so keeping a food diary may help identify what causes issues.
Maintaining a healthy weight, avoiding smoking, and limiting alcohol may also lower headache frequency. Regular exercise, even just a few days a week, can lead to fewer headaches and less severe symptoms. These changes, along with good sleep hygiene, are linked to better control over menstrual and hormone-related headaches, as detailed by the Cleveland Clinic and Mayo Clinic.
Magnesium and Nutritional Support
Magnesium is a mineral that plays a key role in many of the body’s processes, including nerve function and hormone regulation. Some studies suggest that low magnesium levels are linked to more frequent or severe hormonal headaches.
Doctors sometimes recommend magnesium supplements or increasing magnesium-rich foods like spinach, almonds, and pumpkin seeds. It’s important to check with a healthcare provider before starting supplements, as taking too much can cause side effects. In addition to magnesium, a diet with enough vitamins, such as vitamin B2 (riboflavin), may provide extra support against headaches.
Choosing a well-balanced diet rich in nutrients supports overall wellness and may help reduce the frequency and intensity of hormonal headaches, according to Healthline and advice from Northwestern Medicine.
Frequently Asked Questions
Hormonal shifts in women, such as changes in estrogen levels, can lead to headaches that may feel different from other headache types. Treatments, causes, and symptoms often vary depending on age or stage of life.
What are the treatment options for hormonal headaches?
Doctors may suggest over-the-counter pain relievers or prescription medications. In some cases, hormonal therapies, such as birth control pills, are used to balance estrogen levels and help manage symptoms.
Certain lifestyle changes, including regular sleep schedules and stress management, can also help reduce the frequency of hormonal headaches.
Can hormonal changes during perimenopause cause headaches?
Many women experience more headaches during perimenopause due to fluctuating hormone levels. The drop and rise of estrogen and progesterone can trigger headaches during this time.
Medical experts point out that women may notice headaches coming more often or changing in pattern compared to earlier in life.
What are effective home remedies for alleviating hormonal headaches?
Applying a cold pack to the forehead or neck may help reduce pain. Resting in a dark, quiet room can ease headache symptoms for some people.
Staying hydrated, eating balanced meals, and avoiding known headache triggers like caffeine or certain foods might also be helpful.
Does the presence of estrogen or its fluctuation trigger headaches?
Estrogen levels play a significant role in triggering headaches for many women. Headaches often start when estrogen drops sharply, such as before menstruation. This connection is discussed on the Mayo Clinic’s page about headaches and hormones.
Hormonal migraines and other headaches can therefore be closely linked to a woman’s menstrual cycle or hormone changes at other times.
Why might women experience daily headaches during menopause?
During menopause, hormone levels become less stable. This shift can cause some women to experience daily or frequent headaches.
Doctors note that these headaches may be different in severity or frequency from those experienced at other times in life.
Are there specific locations on the head where hormonal headaches manifest?
Hormonal headaches often start on one side of the head and can be moderate to severe. Sometimes, the pain can also include the front or both sides of the head.
Experts say these headaches may get worse with movement, light, smells, or sounds, and this one-sided pain is a common sign of hormonal headaches.
Conclusion
Women hormonal headaches are often linked to changes in estrogen levels. Many women notice headaches become more frequent or severe during menstruation, pregnancy, or menopause. These times bring natural drops or shifts in hormones.
Hormonal headaches can show up as mild or severe pain. They sometimes include symptoms like nausea or sensitivity to light. Some women also experience these headaches after starting or stopping oral contraceptives.
Key factors that affect hormonal headaches include:
- Menstrual cycle phases
- Use of birth control
- Pregnancy and menopause
- Sudden hormone changes
Estrogen drops are a common trigger. Keeping estrogen levels stable may help reduce headache frequency, but this is not always possible for everyone. According to Mayo Clinic, steady estrogen levels can make a difference in headache management.
Doctors may suggest lifestyle changes or medication to help manage these headaches. Headache diaries and identifying triggers are useful tools for many women. Learning about the patterns and causes gives women more control when seeking relief.
For more information on causes and treatments of hormonal headaches, visit Medical News Today and learn how hormonal changes influence symptoms in women's health studies.

