The uterus is a vital organ in a woman’s body, playing an important role in menstrual cycles, fertility, and pregnancy. Good uterine health means the uterus can function as it should, supporting overall reproductive wellbeing. Many conditions, such as fibroids or endometriosis, can affect the uterus and may cause pain, heavy periods, or other symptoms.
Learning about different uterine diseases and how they are diagnosed or treated can help women better understand their bodies and know when to seek medical advice. Taking care of uterine health is key to feeling well and making informed choices about health and future plans.
Key Takeaways
- Uterine health affects periods, fertility, and pregnancy.
- Common conditions include fibroids and endometriosis.
- Early diagnosis and treatment can improve quality of life.
Understanding the Uterus
The uterus, also known as the womb, is a vital organ in the female reproductive system. It plays a direct role in menstruation, pregnancy, and overall reproductive health during a woman's reproductive age.
Functions of the Uterus
The uterus has several important functions related to reproduction. One main role is housing and nourishing a fertilized egg until birth. During pregnancy, the uterus expands and its muscles support the growing baby.
This organ is also involved in the menstrual cycle. Each month, the lining thickens to prepare for a possible pregnancy. If pregnancy does not happen, the lining sheds as menstrual flow.
Other key functions include helping push the baby out during labor and being involved in normal menstrual bleeding. The uterus also interacts with the vagina and cervix, making connections crucial for both fertility and childbirth, as explained by medical experts at the Cleveland Clinic on uterus anatomy and function.
Anatomy and Structure
The uterus is pear-shaped, hollow, and muscular. It is found in the lower abdomen between the bladder and the rectum. The upper part is called the fundus, the main body is the corpus, and the lower part is the cervix.
The cervix connects the uterus to the vagina, acting as a passage for menstrual blood and, during labor, for the baby. The muscular walls let the uterus stretch, contract, and return to its normal size.
There are three layers:
- Perimetrium: The outer layer.
- Myometrium: The thick, muscular middle layer.
- Endometrium: The inner lining that changes during the menstrual cycle.
More detail on these anatomical features is discussed in reliable resources such as the NCBI's statpearls uterus anatomy overview.
Hormonal Regulation of the Uterus
Hormones guide the function and health of the uterus. Estrogen and progesterone are the main hormones that control changes to the uterine lining, especially during the menstrual cycle.
Estrogen helps the endometrium grow and thicken early in the cycle. Progesterone stabilizes and prepares the lining for a fertilized egg in the second half of the cycle. If no pregnancy occurs, hormone levels drop and the lining sheds as a period.
These hormones also affect the cervix and vagina, helping to keep the entire reproductive system healthy. Proper hormone levels are necessary for regular cycles, fertility, and overall uterine health.
Uterine Health and Menstrual Disorders
Problems in the uterus can lead to menstrual changes, pain, or other health concerns. Many women experience symptoms such as heavy bleeding, anemia, or digestive troubles linked to their uterine health.
Heavy and Prolonged Periods
Heavy or long-lasting periods can be a sign of a uterine disorder. Women may soak through pads or tampons in less than two hours, pass large clots, or bleed for more than seven days.
These symptoms are not just bothersome. They can signal problems such as fibroids, adenomyosis, or endometrial polyps. If bleeding is very heavy or lasts a long time each month, it can interfere with normal activities and cause fatigue.
Pain is often present with heavy periods. Some may also have pelvic pain or lower back pain, especially during menstruation. It is important to discuss these symptoms with a healthcare provider, as these issues are outlined in several menstrual disorder guides.
Anemia from Uterine Conditions
Women who have heavy or prolonged periods are at risk for anemia. Anemia means the body does not have enough healthy red blood cells to carry oxygen. Symptoms to look for include:
- Ongoing tiredness
- Weakness
- Pale skin
- Shortness of breath
Low iron levels and anemia can make daily life harder. Sometimes anemia develops slowly, making it harder to notice the symptoms at first. Treating the uterine cause is important, but iron-rich foods or supplements can also help.
Uterine conditions like fibroids and endometriosis often cause the type of bleeding that leads to this problem. Checking blood counts through a simple test can show if anemia is present. For more information on possible causes, read about abnormal menstruation.
Constipation Linked to Uterine Issues
Constipation sometimes happens with uterine disorders. This is often because fibroids or an enlarged uterus press against the bowel. This physical pressure can slow movement in the intestines, making it hard to pass stool.
Women also report stomach bloating, pain in the belly, or feeling full quickly. Sometimes, pain during sex or pelvic pain is present alongside constipation. Certain uterine conditions, like endometriosis, may cause both digestive symptoms and menstrual issues.
For those with lasting constipation and menstrual changes, a healthcare professional should check for possible uterine problems. Information about other common uterine disorders and symptoms can help people understand when to get help.
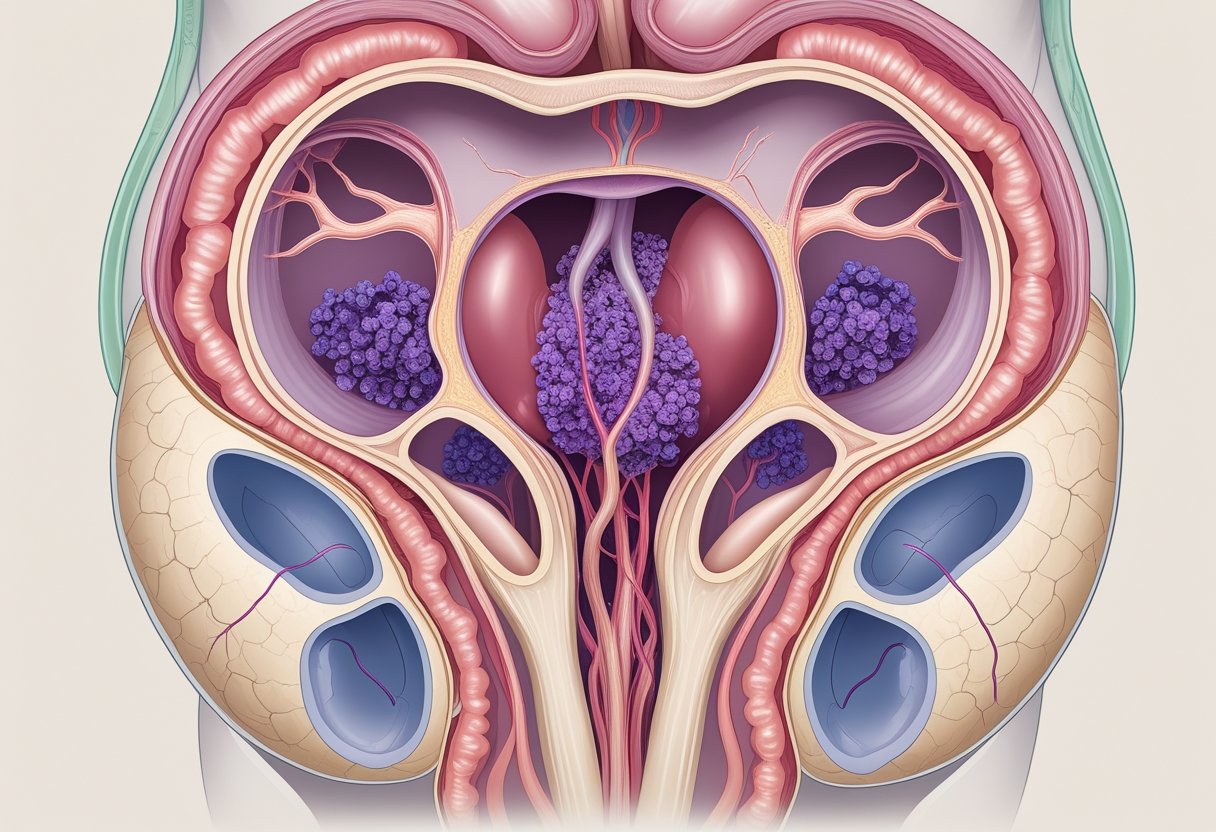
Uterine Fibroids and Benign Growths
Uterine fibroids are noncancerous tumors that develop in or on the uterus. These growths, also called leiomyomas or myomas, affect many people with a uterus and can appear in several forms with different symptoms.
Types of Fibroids
Fibroids can vary in size, shape, and location. They are usually classified by where they are found in the uterus:
- Intramural fibroids: These grow within the muscular wall of the uterus and are the most common type.
- Subserosal fibroids: These develop on the outside wall of the uterus.
- Submucosal fibroids: These form just under the lining of the uterus and may extend into the uterine cavity.
- Pedunculated fibroids: These are attached to the uterus by a thin stalk.
Most fibroids are benign and do not turn into cancerous growths. They often develop as single tumors, but sometimes multiple fibroids can grow at the same time. Learn more about how uterine fibroids are non-cancerous.
Symptoms of Uterine Fibroids
Some people with fibroids have no symptoms, especially if the fibroids are small. When symptoms do appear, they depend on the size, location, and number of fibroids.
Common symptoms include:
- Heavy or long menstrual periods
- Pelvic pain or pressure
- Frequent urination
- Trouble emptying the bladder
- Pain during sex
In some cases, fibroids may also cause lower back pain or leg pain if they press on nerves. The presence of multiple or large fibroids can sometimes lead to swelling in the lower abdomen. For more information on symptoms of uterine fibroids, consult a healthcare provider.
Uterine Cancer and Malignancies
Uterine cancer develops when cells in the uterus grow in an uncontrolled way. The main types include endometrial cancer and other gynecologic cancers. Early diagnosis and treatment can improve outcomes for most cases.
Endometrial Cancer
Endometrial cancer is the most common type of uterine cancer. It begins in the lining of the uterus called the endometrium. Most cases are found in women who have gone through menopause.
A leading sign is abnormal vaginal bleeding, such as bleeding between periods or after menopause. Doctors will often use a biopsy to check for cancer. They may also use imaging tests like ultrasounds or MRIs to see how far the cancer has spread.
Treatment usually involves surgery to remove the uterus (hysterectomy). Sometimes, radiation therapy or chemotherapy is needed.
Risk factors for endometrial cancer include obesity, hormone imbalance, diabetes, and family history. Women who notice unusual bleeding should talk to their doctor right away. For more details, see the page on endometrial cancer symptoms and causes.
Gynecologic Cancers
Other gynecologic cancers affecting the uterus include less common forms like uterine sarcoma. Sarcomas start in the muscles or tissues of the uterus, not the lining. Cervical cancer is a separate gynecologic cancer that affects the cervix, not the uterus, but it can have some overlapping symptoms like abnormal bleeding.
Doctors diagnose these cancers with a combination of pelvic exams, imaging tests, and tissue samples. Treatment options depend on the type and stage of the cancer. They may include surgery, radiation, chemotherapy, or a mix.
Timely diagnosis and treatment are important. Regular check-ups and discussing symptoms help catch cancers earlier. Learn more about different types of gynecologic cancers including uterine cancer.
Other Uterine and Pelvic Disorders
Uterine and pelvic disorders often affect women’s daily comfort and long-term health. Understanding the unique features and symptoms can help with early recognition and proper care.
Endometriosis and Polyps
Endometriosis happens when tissue similar to the lining of the uterus grows outside of it. This can cause intense pain, heavy periods, and even infertility. Common pain spots include the lower belly and pelvis. Some women also notice pain when using the bathroom or during sexual activity.
Treatment options for endometriosis may include pain medicine, hormone therapy, or surgery. Early diagnosis and proper care can help reduce symptoms and protect fertility.
Polyps are small growths inside the uterus. These may lead to irregular bleeding, spotting between periods, or trouble getting pregnant. Polyps can be found by ultrasound or hysteroscopy and are often removed if they cause problems. Details on these conditions are available at MedlinePlus and UT Southwestern Medical Center.
Pelvic Inflammatory Disease and Scarring
Pelvic Inflammatory Disease (PID) is an infection of the female reproductive organs. Sexually transmitted bacteria can travel from the vagina to the uterus, fallopian tubes, or ovaries. Symptoms often include pain in the lower abdomen, abnormal discharge, fever, and pain during sex.
Untreated PID can cause scarring inside the uterus or fallopian tubes. Scarring increases the risk of long-term pelvic pain and makes it harder to get pregnant. Treatment usually involves antibiotics to stop the infection. Early treatment can help prevent permanent damage.
Warning Signs to Watch For:
- Persistent pelvic pain
- Unusual discharge
- High fever
Seek medical attention quickly if these symptoms appear.
Polycystic Ovary Syndrome
Polycystic Ovary Syndrome (PCOS) affects hormone levels and the way ovaries work. Women with PCOS may have irregular menstrual cycles, extra hair growth, or acne. The ovaries may become enlarged and develop many small cysts.
PCOS is one of the leading causes of infertility. It is also linked to a higher risk of diabetes and heart problems. Managing PCOS often involves lifestyle changes, such as healthier eating, physical activity, and sometimes medicines to balance hormones or help with fertility.
For more details, visit the section about common reproductive health concerns.
Symptoms and Diagnosis of Uterine Conditions
Uterine health issues can cause changes in bleeding, pain, and other symptoms. Early and accurate diagnosis depends on a mix of patient history, physical examination, and various tests.
Common Symptoms
The most frequent symptoms of uterine problems include:
- Heavy menstrual bleeding
- Pelvic pain or pressure
- Irregular periods
- Bleeding between periods
- Pain during sex
- Pain during urination or bowel movements
Some people also have swelling or bloating in the lower belly. In certain cases, especially with conditions like fibroids or endometriosis, symptoms can disrupt daily life and may even make it hard to get pregnant. Symptoms can also depend on the specific condition, for example, uterine fibroids, polyps, or cancer. Uterine cancer might cause bleeding after menopause, which should always be checked by a doctor. For a more detailed list and descriptions of symptoms, visit this uterus problems guide.
Pelvic Examination
A pelvic exam is often the first step a doctor takes to check for uterine problems. During this exam, the doctor looks at and feels the uterus, ovaries, and nearby areas to check for any swelling, tender spots, or abnormal growths.
The exam can help the doctor find clues about the condition, such as if the uterus feels bigger than normal, is less flexible, or if there are lumps. Sometimes, the doctor can feel fibroids or cysts during the exam. If anything unusual is found, more tests may be ordered.
The pelvic examination is quick and does not usually cause much pain, but it might feel a little uncomfortable.
Imaging and Diagnostic Tests
Doctors use imaging tests to see inside the uterus and confirm a suspected condition. An ultrasound is a common test that uses sound waves to help spot fibroids, cysts, or other growths. This test is usually painless and can show the size and shape of the uterus.
Other imaging methods include MRI and CT scans for more detailed pictures. For a close-up look inside the uterus, a hysteroscopy may be done. This involves a tiny camera that goes through the vagina into the uterus so doctors can see polyps or scar tissue.
A laparoscopy is another procedure that allows doctors to see the uterus and pelvic organs through small cuts in the belly. This test is often used to find endometriosis or other problems that cannot be seen with ultrasound. For more on these diagnostic tools, see this guide to common uterine conditions.
Impact on Fertility and Pregnancy
Common problems with the uterus can lower a woman's chance of getting pregnant or having a healthy pregnancy. Fibroids, polyps, or a misshapen uterus may lead to issues like trouble conceiving, higher risk of miscarriage, or pregnancy complications including preterm birth.
Infertility and Miscarriage
Studies show fibroids are present in about 5-10% of women who struggle to get pregnant. In some cases, fibroids may be the only cause of a woman's infertility. These growths can block the uterus or change its shape, making it harder for an embryo to implant. Polyps and severe adhesions, also known as scar tissue, can have a similar effect.
A uterus with abnormal structure, such as septate or bicornuate uterus, can increase the risk of miscarriage. Poor uterine lining can also play a part if the lining is too thin or not healthy enough for an embryo to grow. Infections and chronic inflammation may lead to repeated pregnancy loss as well.
For more information about uterine factors and their impact on infertility, see how uterine abnormalities affect fertility and the connection between fibroids and infertility.
Pregnancy Complications
Once pregnancy begins, some uterine conditions can raise the risk of problems. Women with large or multiple fibroids have a higher chance of preterm labor, abnormal position of the baby (such as breech), or problems with the placenta. Heavy bleeding and pain can also occur, which may require special care.
Adhesions (scar tissue) from previous surgery or infection can cause the uterus to stretch unevenly during pregnancy. This might lead to decreased growth for the baby or trouble with the placenta. Abnormal shapes of the uterus, like bicornuate or unicornuate uterus, make it more likely for the baby to be born early or for the pregnancy to end up in miscarriage.
Understanding these risks is important because it can help women and their doctors watch for problems early during pregnancy. Detailed information is available on pregnancy risks associated with uterine fibroids.
Treatment and Management Options
Treatment for uterine health conditions often depends on the type and severity of the issue. Surgical and medical therapies are available, and lifestyle choices can affect recovery and risk of future problems.
Surgical Treatments for Uterine Conditions
Surgical options can be important for treating moderate or severe uterine problems. Hysterectomy, which removes the uterus, is one of the most common surgeries. It is often chosen when other treatments fail or when symptoms are severe. Women who have a hysterectomy cannot become pregnant afterward.
Myomectomy is a surgery that removes only fibroids, leaving the uterus intact. This is a good option for those who want to keep their fertility. Another treatment, uterine artery embolization, blocks blood flow to fibroids, causing them to shrink.
Dilation and curettage (D&C) is used to remove tissue from the uterus. It treats heavy bleeding, removes polyps, or evaluates abnormal cells. Surgical risks include infection, bleeding, or complications with future pregnancies. Recovery time and side effects depend on the procedure. For more details on these options, visit this guide to uterine fibroid treatments.
Medical and Non-Surgical Therapies
Many uterine conditions can be managed with medication. Hormonal therapies, such as oral contraceptives or progestins, help control heavy bleeding or pain. Medicines that affect hormones like GnRH agonists can shrink fibroids and ease symptoms.
Non-surgical therapies also include newer oral medications, like elagolix. These drugs manage bleeding from fibroids in people who have not reached menopause. Pain relievers and anti-inflammatory drugs can reduce mild symptoms. In some cases, intravenous estrogen or hormone therapy may be used for acute bleeding.
Some therapies have side effects such as hot flashes, bone thinning, or changes to menstrual periods. The choice of therapy depends on a person’s age, symptoms, desire for children, and health history. Read more about medication and therapy for uterine conditions at this medical overview.
Lifestyle Factors Affecting Uterine Health
Weight, diet, and general health can directly affect the uterus. Obesity increases the risk of many uterine problems, such as fibroids and endometrial hyperplasia. A healthy weight can lower these risks.
Conditions like diabetes also play a role. Unmanaged diabetes can change hormone levels and raise the risk of endometrial cancer. High levels of male hormones (androgens) in women may disrupt the menstrual cycle and affect uterine health.
Menopause naturally reduces some risks but can increase others, such as urinary or tissue changes. Healthy habits like regular exercise, balanced nutrition, and not smoking may support better uterine function. Annual check-ups help catch problems early and improve long-term health.
Frequently Asked Questions
Uterine health can be influenced by physical symptoms, personal habits, and specific nutrients. Early recognition and daily care play important roles in fertility, menstruation, and disease prevention.
What are common indications of an unhealthy uterus?
Common signs of an unhealthy uterus include abnormal vaginal bleeding, irregular or painful periods, and pelvic pain. Some people experience pain during intercourse or have difficulty becoming pregnant. Swelling, frequent urination, or persistent lower belly pressure may also be noticed.
Which supplements are beneficial for maintaining a healthy uterus?
Folic acid is important for women of childbearing age as it helps support overall reproductive health. Iron and vitamin D may help maintain healthy blood and tissues. Omega-3 fatty acids can decrease inflammation, and some people also use magnesium or calcium.
What are the primary diseases that can affect the uterus?
Uterine fibroids, which are non-cancerous growths, are common and may cause heavy periods or pain. Endometriosis is another disease that causes tissue similar to the uterine lining to grow outside the uterus. Uterine cancer and adenomyosis are also recognized uterine disorders. More information about fibroids can be found at the UCLA Health fibroid FAQ page and uterine cancer details at the Henry Ford Health uterine cancer FAQ.
How can lifestyle changes contribute to uterine health?
Maintaining a healthy weight lowers the risk of developing some uterine disorders. Regular exercise and eating a balanced diet can help control hormone levels. Avoiding smoking and limiting alcohol may also protect uterine tissues.
In what ways can herbal teas support uterine well-being?
Some herbal teas, such as raspberry leaf and chamomile, are believed to soothe menstrual discomfort. Ginger tea may reduce inflammation and cramping. Always consult a health provider before using herbal products, as some herbs can interact with medications.
What preventative measures can be taken to avoid uterine disorders?
Routine gynecological exams and screenings can help detect problems early. Practicing safe sex and managing chronic illnesses may decrease risk. Eating a diet high in fruits, vegetables, and whole grains can also support uterine health and lower inflammation.
Conclusion
Maintaining uterine health helps protect comfort, fertility, and quality of life. Regular checkups and open communication with healthcare providers can help many women spot issues early. Some common problems include fibroids, endometriosis, and uterine prolapse.
Key Factors Supporting Uterine Health:
- A balanced diet
- Regular physical activity
- Avoiding smoking or excessive alcohol
- Managing stress
Fibroids are one of the most common concerns. They can cause pain, bleeding, and sometimes affect fertility. Women often worry about treatment options, especially surgical ones, for uterine leiomyomas (fibroids).
Environmental factors, like exposure to toxins, may also impact the uterine environment. This can influence fertility or embryo health, as toxins such as cigarette smoke can harm the uterus.
As women get older, the risk for certain uterine conditions can rise, including cancer and endometrial changes. Routine screenings are important to catch problems early.
Learning about symptoms, staying informed about treatment choices, and seeking care when needed all support better uterine health.

