Hormonal acne is a common skin problem that affects both teens and adults, and is often caused by changes in hormone levels. This type of acne tends to flare up at certain times, like around menstrual periods, puberty, or during stressful times, and is usually found along the jawline, chin, and lower face. It can be frustrating because it sometimes does not respond to regular acne treatments.
Many people find hormonal acne difficult to understand because the triggers can be different from person to person. For example, it may be linked to hormonal changes, stress, certain medications, or underlying health conditions. Knowing what sets off these breakouts is important for anyone who wants clearer skin and fewer flare-ups.
Key Takeaways
- Hormonal acne is linked to changes in hormone levels
- Triggers and symptoms vary from person to person
- Different treatments can help manage and prevent breakouts
Understanding Hormonal Acne
Hormonal acne often appears when hormone levels in the body change or fluctuate. These shifts can lead to several types of blemishes that affect people of different ages.
What Is Hormonal Acne?
Hormonal acne is a skin condition caused by changes in hormone levels in the body. It is common among teenagers, but many adults experience it too. Women between ages 20 and 50 are especially likely to see breakouts from hormone changes, such as those during periods, pregnancy, or menopause.
This type of acne often includes whiteheads, blackheads, papules, pustules, cysts, or nodules. Unlike regular acne, hormonal acne tends to appear along the lower face, jawline, and chin. Adult acne flare-ups happen when oil glands make too much sebum, which can clog pores and trigger inflammation. For more detailed information, see this overview of hormonal acne.
Hormonal Imbalance and Acne
Hormonal imbalances play a key role in causing acne. Androgens, such as testosterone, make the oil glands work harder. When androgen levels rise, so does oil production, leading to clogged pores and acne-prone skin. Estrogen and progesterone, which also change during the menstrual cycle, can trigger pimples for many women.
Fluctuations in these hormones can happen because of puberty, stress, certain medications, or changes related to aging. Sometimes, medical conditions like polycystic ovary syndrome (PCOS) can cause long-term hormonal imbalances. Such changes in hormone levels are a major reason why some adults still get acne, especially women. Learn more about the connection between hormonal imbalance and acne.
Common Symptoms of Hormonal Acne
Hormonal acne comes with certain symptoms that set it apart from regular pimples. The breakouts often occur on the lower part of the face, including the jaw, chin, and cheeks. The most common types of blemishes are:
- Whiteheads and blackheads
- Papules (small red bumps)
- Pustules (pimples with pus)
- Cysts and nodules (painful lumps deep under the skin)
Some people also notice their acne gets worse around their menstrual period or when under stress. Severe cases may leave scars or dark marks even after the pimples heal. Hormonal acne is often stubborn and may require targeted treatments from a dermatologist. Find out more about the symptoms and scarring risk.
Causes of Hormonal Acne
Hormonal acne is linked to changes in hormone levels that can affect oil production in the skin. Genetics, life stages, and family history also play a part in who gets hormonal acne and when it is most likely to occur.
Role of Hormones and Androgens
Hormonal acne often develops when levels of certain hormones, especially androgens, increase in the body. Androgens such as testosterone can make the skin produce more oil (sebum). Too much sebum can clog pores and lead to pimples or cysts.
Androgen levels rise during puberty in both boys and girls. This is why teens often get more acne. In adults, small changes in hormones like estrogen and progesterone can also affect sebum production.
Stress can impact hormone levels, making acne worse. Medical conditions that raise androgen levels, such as polycystic ovary syndrome (PCOS), may also trigger more frequent breakouts. For more information about how hormones drive acne, visit this detailed explanation of hormone triggers.
Influence of Genetics and Family History
A person is more likely to develop hormonal acne if close family members also had it. Genetics influence how the skin responds to hormones and how much oil it produces. If parents or siblings had severe or persistent acne, the chances of experiencing similar problems increase.
Certain genes may affect how sensitive the skin is to androgens, leading to more clogging of hair follicles and more acne. Genetics can also impact inflammation levels in the skin, making breakouts more severe for some individuals.
Family history does not guarantee acne, but it does raise the risk. Genetics help explain why some people struggle with acne even when they follow a good skincare routine.
Hormonal Fluctuations During Life Stages
Hormonal changes during key life stages can have a strong effect on acne development. Puberty is a common time for acne because androgens increase and boost sebum production. But hormonal acne is not limited to teens.
Many women see new or worse acne around their menstrual cycle, when hormone levels shift. Pregnancy can also change estrogen and progesterone levels, which may trigger breakouts or clear acne, depending on the person.
Acne may appear or get worse during perimenopause and menopause, mainly because of changes in hormone balance. These shifts in estrogen and progesterone can again increase oil production and clog pores. For more details on how life stages impact acne, see this overview of acne and hormonal changes.
How Hormonal Acne Develops
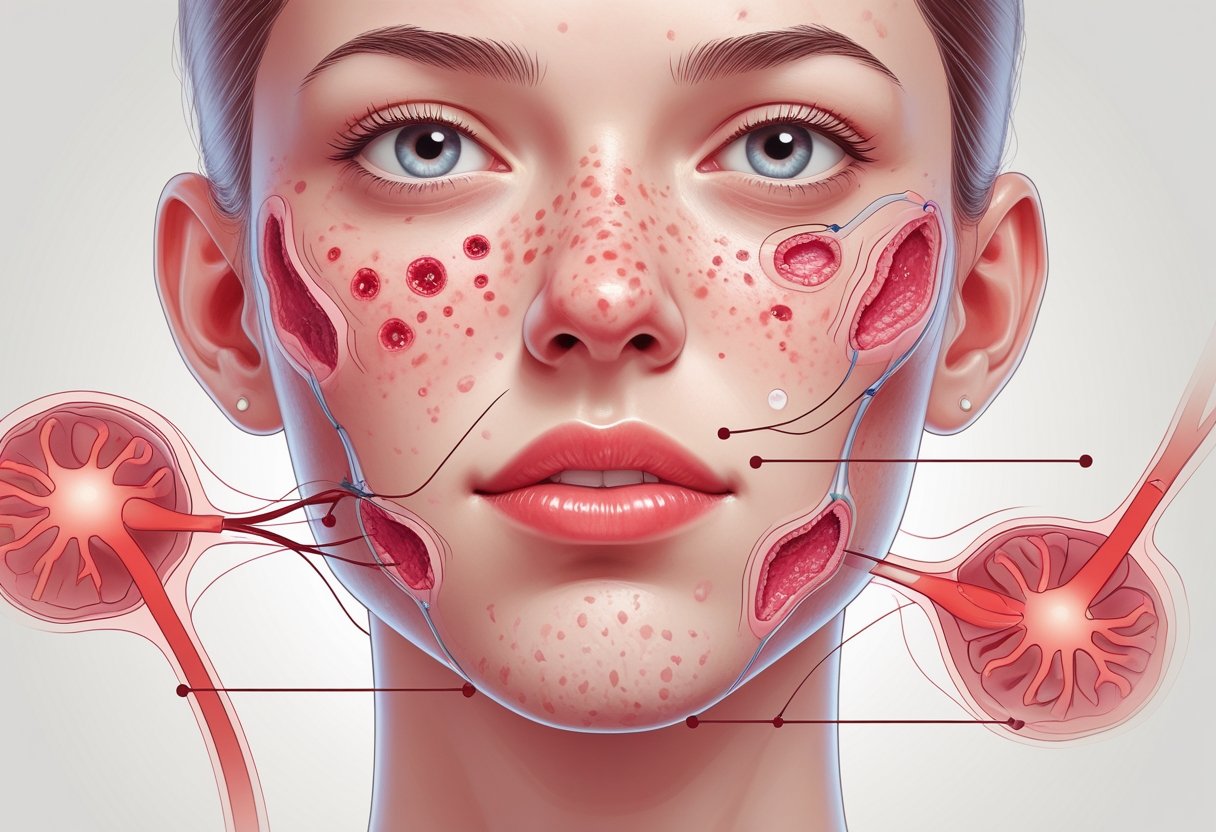
Hormonal acne begins when hormone levels change and cause the oil glands in the skin to produce more sebum. This extra oil, combined with dead skin cells and bacteria, can lead to blocked pores, infection, and inflammation.
Sebum Production and Oil Glands
Sebaceous glands are small glands found in the skin, usually near hair follicles. These glands make sebum, an oily substance that helps keep the skin moist and protected. During puberty or other hormone shifts, hormones like testosterone can cause the sebaceous glands to make too much sebum.
When sebum production increases, oil collects on the skin's surface. If there is too much oil, it mixes with dead skin cells in the pores. Excess oil can worsen the chances of clogged pores and is a common trigger for breakouts, especially in areas with more oil glands like the face, back, and chest. To learn more about how overproduction of sebum leads to acne, visit this page on hormonal acne and oil glands.
Clogged Pores and Bacterial Growth
When too much sebum mixes with dead skin cells, it can block or clog the hair follicles. These clogged pores trap oil and debris inside the follicle. The blocked pore creates an environment where acne-causing bacteria called Cutibacterium acnes can grow quickly.
As the bacteria multiply, they use the trapped sebum as food. The buildup inside pores forms whiteheads, blackheads, and sometimes deeper bumps. Clogged pores are a main reason that acne gets worse for people with hormonal changes, especially when there is extra oil and dead skin cells. More information about pore blockage and bacterial growth in acne can be found in this Medical News Today article.
Inflammation and Immune Response
The body's immune system sees the growing bacteria and blocked pores as a problem. White blood cells rush to the area to fight the bacteria, leading to inflammation. This causes redness, swelling, and pain in the affected spots.
The inflammation can damage the surrounding skin tissues, sometimes leaving scars if the infection goes deep. Products of the immune reaction, like pus, may also collect, forming pimples or cysts. The cycle continues when the immune system keeps attacking new spots, which is why hormonal acne can last for a long time and flare up from time to time.
Identifying Types and Severity of Hormonal Acne

Hormonal acne presents in several distinct ways, affecting both the appearance of the skin and a person’s quality of life. The severity and type of acne can help guide treatment options and predict outcomes such as scarring or discoloration.
Common Lesions and Their Presentation
Hormonal acne often includes several types of lesions: blackheads, whiteheads, papules, pustules, nodules, and cysts. Blackheads and whiteheads are known as comedones. Blackheads are open at the surface and appear dark, while whiteheads are closed and have a white tip.
Papules are small, red bumps that can be sensitive to touch. Pustules are similar but filled with pus. Severe cases include deep, painful nodules and cysts that form under the skin and may last for weeks. These can result in more significant acne scarring and marks, including post-inflammatory hyperpigmentation. Cystic and nodular acne signal a more advanced and difficult-to-treat condition, often requiring medical intervention. For more details on what these lesions look like, see this description of hormonal acne types and presentations.
Hormonal Acne in Adults vs. Teenagers
Hormonal acne affects teenagers and adults differently. During puberty, teens often develop blackheads, whiteheads, and other comedones along the forehead and nose. Hormone changes spike at this age, leading to common and widespread breakouts.
Adults, especially women, may see more cystic and nodular acne along the chin, jawline, and lower cheeks. Adult acne can be linked to menstruation, pregnancy, or conditions like polycystic ovary syndrome. Unlike teen acne, adult breakouts are deeper and last longer, and they may be more likely to leave behind dark spots or scars. These differences between ages are important when choosing treatments. Read more about how hormonal acne varies by age.
Associated Symptoms and Complications
Severe hormonal acne can cause more than just blemishes. Painful cysts and nodules may lead to long-term scarring or areas of post-inflammatory hyperpigmentation, especially in darker skin types. Some people also develop itching, tenderness, or swelling around acne lesions.
Physical symptoms sometimes come with emotional distress, including low self-confidence and anxiety about appearance. In adult women, hormonal acne sometimes appears along with other signs of hormonal imbalance, such as changes in facial hair or menstrual cycles. If acne is persistent or causes scarring, medical advice should be sought to help prevent further complications. Learn about the risks of scarring and complications linked to severe hormonal acne.
Triggers and Risk Factors
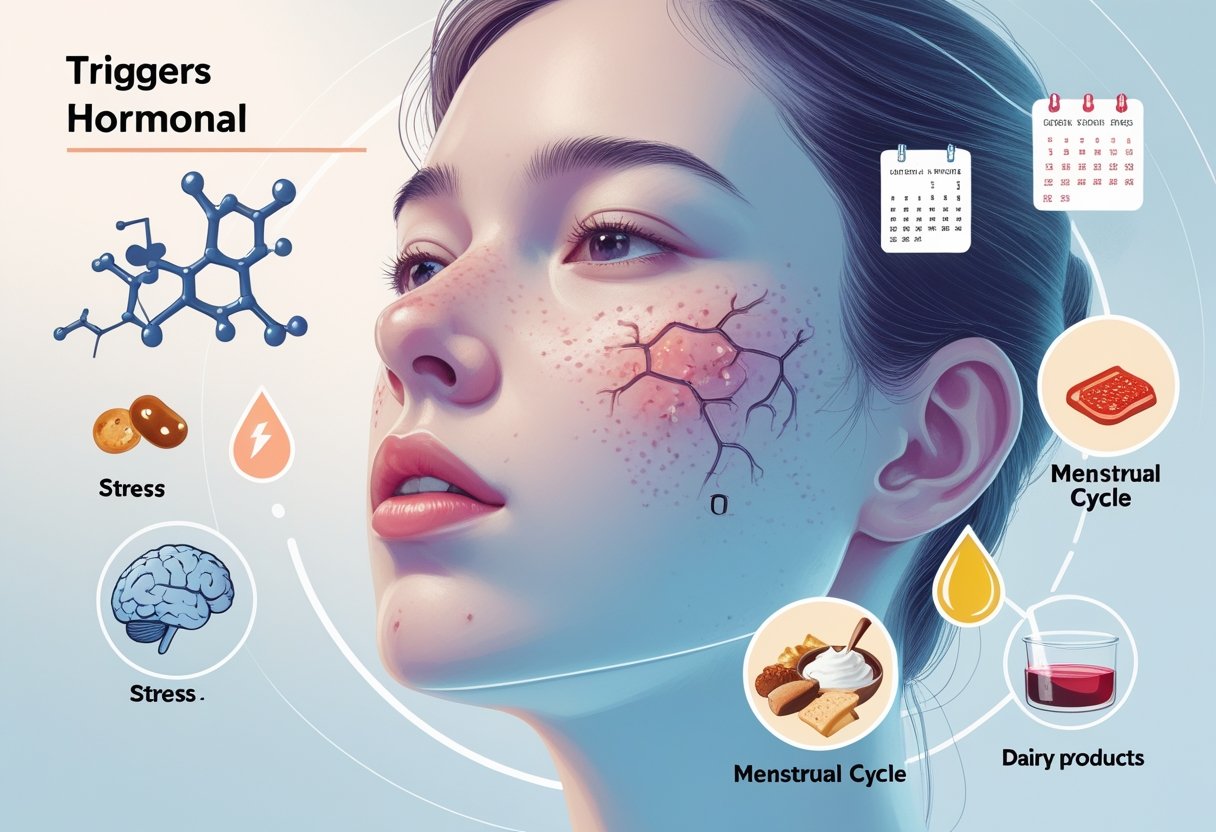
Several factors can make hormonal acne worse. Stress, certain foods, and health conditions can increase the chance of breakouts or make acne more difficult to treat.
Impact of Stress and Lifestyle
Rising stress levels increase the body's production of hormones such as cortisol. Extra cortisol can lead to more oil (sebum) in the skin. When pores get blocked with this extra oil, breakouts are more likely.
A busy lifestyle, lack of sleep, and irregular routines can all make stress worse. Teens and adults with busy schedules may notice more acne during intense work or study periods. Lifestyle changes like regular exercise, getting enough sleep, and good hygiene may lower stress and help prevent flare-ups.
Healthy habits also matter. Smoking, using harsh skin products, or touching the face too often can cause more skin irritation. Reducing these habits is helpful for those who want clearer skin.
Diet and Dairy Intake
Certain foods may impact hormonal acne for some people. Diets high in sugar and processed foods can raise insulin, a hormone that sometimes triggers more oil production. Foods that cause fast changes in blood sugar may increase the chance of acne.
Dairy intake, especially skim milk, has been linked by multiple studies to higher rates of acne. The hormones in cow's milk, even after processing, may affect hormone levels in the body. Not everyone is sensitive to dairy this way, but cutting back on milk and cheese may help some people.
Eating a balanced diet with whole grains, lean proteins, fruits, and vegetables supports better skin. Staying hydrated and limiting junk food can also make a difference.
Medical Conditions Affecting Hormonal Acne
Some health problems can make hormonal acne worse. One of the most common is polycystic ovary syndrome (PCOS). PCOS leads to increased levels of androgens, a type of hormone that raises oil production and often causes severe acne in women.
Other hormone disorders, thyroid issues, or sudden weight gain can increase the risk of breakouts. Medications that change hormone levels may cause acne as a side effect.
Women may also notice acne flare-ups before their periods, during pregnancy, or after stopping birth control, when hormone levels shift. These changes make certain times in life more prone to breakouts. For more details about hormonal causes, visit this page on hormonal causes and acne.
Diagnosing Hormonal Acne
Hormonal acne is often recognized by its pattern, location, and type of lesions. Diagnosis usually involves a physical exam and questions about medical history.
Clinical Evaluation and Medical History
A dermatologist will examine the skin to look for specific signs of hormonal acne. Common areas include the lower face, jawline, and neck. Types of spots such as whiteheads, blackheads, papules, pustules, and sometimes cysts or nodules may be present.
The doctor will ask about age, menstrual cycle changes, stress levels, and any skin care products used. A full skin examination is done on the face, chest, and back to check for multiple types of blemishes. Most cases do not need special lab tests. A clear diagnosis helps guide a targeted skin care regimen.
Treatment Options for Hormonal Acne
Hormonal acne can be managed with a range of treatments. These include skin creams, oral medications, and procedures done by healthcare professionals.
Topical Treatments
Topical treatments are the first step for many people with hormonal acne, especially if the acne is mild to moderate. Creams and gels with ingredients like benzoyl peroxide, salicylic acid, and azelaic acid help to clear blocked pores and reduce inflammation. Benzoyl peroxide kills bacteria and can lower swelling, while salicylic acid works by exfoliating the skin and keeping pores clear.
Topical retinoids, such as adapalene, are also common. They help reduce the buildup of skin cells and oil. Retinoids need to be used regularly, and sometimes the skin can feel dry or irritated at first. It is important to pick products labeled as non-comedogenic so they do not block pores further. In some cases, a doctor may prescribe a newer topical treatment called clascoterone, which helps control hormones in the skin.
| Treatment | Main Action |
|---|---|
| Benzoyl Peroxide | Kills bacteria |
| Salicylic Acid | Exfoliates, unblocks pores |
| Azelaic Acid | Reduces redness |
| Adapalene/Retinoids | Prevents clogged pores |
| Clascoterone | Reduces hormone action |
Oral Medications and Hormonal Therapy
When topical treatments do not work well, oral medications or hormonal therapy may be used. Oral antibiotics help reduce redness and bacteria but are only for short-term use because of side effects and the risk of resistance. Isotretinoin is a strong medication often used for severe cases. It works well but needs doctor supervision because of possible side effects.
Hormonal therapy is another option for people with acne tied to hormones. Some use birth control pills or medicine like spironolactone, which helps block the effects of certain hormones that cause oil gland activity. Spironolactone is usually used for women with persistent or severe hormonal acne. Hormonal therapies may take a few months to show improvement. Patients should talk to a healthcare provider about risks and benefits.
In-Office Medical Treatments
Some people may need in-office medical treatments if their acne does not get better with creams or pills. Chemical peels can help by removing the top layer of skin, which often decreases acne and improves overall skin texture.
Photodynamic therapy uses special lights to target the bacteria and oil glands that cause acne. Another option is ablative laser treatments. These treatments remove damaged skin and decrease oil production, which can lead to fewer breakouts.
A dermatologist can recommend which procedure is best based on the individual’s needs. Medical treatments are often combined with home options for best results. Some treatments may cause redness or mild discomfort for a few days after the procedure. More than one session may be needed for lasting effects. For more information, check Cleveland Clinic’s guide on hormonal acne treatment options.
Long-term Management and Prevention
Long-term control of hormonal acne relies on daily habits and recognizing individual triggers. Consistency with skin care and lifestyle changes can make breakouts less frequent and less severe for most people.
Establishing an Effective Skincare Routine
A good skin care regimen starts with gentle cleansing twice each day. This helps remove oil, sweat, and dirt that could clog pores. Non-comedogenic cleansers and moisturizers are best, as they do not block pores.
Using* acne-fighting ingredients** is important. Products with benzoyl peroxide, salicylic acid, or adapalene target blocked pores and inflammation. Sunscreen is also needed every morning, even on cloudy days. Exposure to the sun can make acne worse and increase the risk for post-acne marks.
Applying all products with clean hands and avoiding harsh scrubs can prevent irritation. Sticking to a set routine helps support clear skin and keeps new breakouts from forming.
Monitoring Triggers and Preventive Measures
Some daily habits or foods may trigger hormonal acne for certain people. Common triggers include high-sugar foods, dairy, and stress. Keeping a journal of breakouts and daily habits can help find patterns over time.
Lifestyle changes matter. A balanced diet with plenty of fruits, vegetables, and water may help reduce breakouts. Regular physical activity and getting enough sleep also support skin health. Managing stress with mindfulness or relaxation exercises can lower hormone swings that often make acne worse.
If acne does not improve with these steps, it is best to talk with a dermatologist. They may recommend prescription treatments or further changes, such as those reviewed by Cleveland Clinic and Healthline.
When to Seek Professional Help
Hormonal acne can sometimes be managed at home, but there are clear signs when seeing a dermatologist is the best choice. Recognizing these symptoms and taking action early may help prevent scarring and long-lasting skin damage.
Indications for Seeing a Dermatologist
People should consider a dermatologist if their acne is severe, painful, or forms cysts and nodules. These types of breakouts do not usually get better with simple or over-the-counter acne treatment. Cystic acne can last for weeks or even months and often returns.
Other important reasons to seek help include persistent acne that lasts for more than a couple of months, visible scarring, or if the acne is causing emotional distress, such as low self-esteem. A dermatologist may recommend advanced treatments, including prescription creams or oral medications, if basic options have failed. Early treatment can lower the chance of permanent scarring and social discomfort, as noted by experts.
Frequently Asked Questions
Hormonal acne can be managed through a mix of medical treatments, lifestyle choices, and dietary changes. Certain foods and habits can make symptoms worse, while effective care can help reduce breakouts.
What are effective treatments for hormonal acne?
Prescription medications like birth control pills, spironolactone, and retinoids are often recommended by doctors for hormonal acne. Over-the-counter creams with benzoyl peroxide or salicylic acid may also help, especially for mild cases.
In some cases, dermatologists suggest stronger options or light-based therapies. Treatment depends on acne severity and underlying hormone issues. Learn more about treatments for hormonal acne.
How can hormonal acne be managed naturally at home?
Gentle skin care is important. Use a mild cleanser, keep skin moisturized, and avoid picking at pimples. Applying ice may reduce swelling.
Some people find that reducing stress, getting enough sleep, and keeping a regular face washing routine helps limit breakouts. Natural remedies do not work for everyone, but they are easy to try and generally safe.
Which dietary changes may improve hormonal acne?
Eating foods with a low glycemic index, like whole grains and vegetables, may help lower acne risk. Some studies suggest cutting back on sugar and dairy could improve symptoms for some people.
Staying hydrated and eating more fruits and vegetables are recommended. Everyone's skin is different, so changes may need some trial and error.
What are the common causes of hormonal acne?
Hormonal acne is usually caused by changes in hormone levels, especially androgens like testosterone. These shifts can increase oil production and clog pores.
Hormonal changes are common during puberty, menstrual cycles, pregnancy, and menopause. Stress and some medical conditions can also affect hormone balance. For more information on causes, visit this guide on common causes of hormonal acne.
Can hormonal imbalance affect skin health, and how to address it?
Yes, hormone imbalances can lead to extra oil on the skin, causing breakouts and pimples. Doctors may check for hormonal problems if acne is severe or does not improve with basic care.
Treatment might include hormone therapy or medications that target hormonal issues. Talking to a healthcare provider is the best way to address hormone-related acne.
Are there any foods known to exacerbate hormonal acne?
Foods high in sugar and processed carbs, such as candy, white bread, and soda, may make hormonal acne worse. Some studies link dairy, especially skim milk, to higher rates of breakouts.
Eating more fruits, vegetables, and whole grains may be helpful, while limiting sugary and high-fat foods could reduce flare-ups. More info is available in this FAQ about acne and diet.
Conclusion
Hormonal acne affects many people, especially women between the ages of 20 and 50. Fluctuations in hormones, such as androgens, are a major cause. These changes often happen during times like menstruation, pregnancy, or menopause.
Many find that sleep disruption can impact their skin. Poor sleep might lead to increased stress and hormonal shifts, which can make acne worse.
Treatment plans often combine lifestyle changes, skin care, and sometimes medication. It is important for individuals to be patient, as improvement can take time.
Common approaches include:
- Gentle cleansing routines
- Consistent sleep schedules
- Healthy diets low in sugar
- Use of prescribed topical or oral medications
People dealing with hormonal acne should talk with a healthcare provider to find what works best for them. Getting enough rest and managing stress may also support clearer skin.
To learn more about causes and treatments, see this guide on hormonal acne.

