Breast health is an important part of overall wellness for people of all ages. Understanding what is normal for your body helps you notice changes early and take action if needed. Staying informed about breast health can help lower risks and give peace of mind.

Regular self-checks, clinical exams, and mammograms are key tools to support breast health. Learning what steps to take and when can make a real difference for early detection and prevention. Reliable programs, such as the Northwestern Medicine Breast Health Program, offer support, guidance, and expert care for those seeking more information or assistance.
Key Takeaways
- Breast health awareness helps with early detection.
- Routine screening and modern diagnostic tools are important.
- Knowledge and support can guide treatment and recovery.
Understanding Breast Health
Good breast health starts with knowing how the breasts work, possible health problems, and the things that can increase the risk of developing breast cancer or other conditions. Women of all ages should learn what is normal for their bodies and how their health may change over time.
Breast Anatomy and Function
The female breast is made up of lobules (milk-producing glands), ducts (tubes carrying milk to the nipple), fatty tissue, and connective tissue. The areola is the dark area around the nipple. Breasts also contain blood vessels and lymph nodes, which are part of the body's immune system.
Breast tissue changes through different stages of life. During puberty, the breasts develop and grow. Hormones like estrogen and progesterone make the breast tissue more sensitive and shape its structure. Pregnancy and breastfeeding can cause further changes due to increased hormone levels.
Understanding the structure of the breast helps people recognize when something feels different, which is important for spotting problems early. The tissue can also feel different depending on the menstrual cycle, which is normal and not usually a cause for concern. For more information on how breast tissue is made and works, see UCSF Health’s education on basic facts about breast health.
Common Breast Conditions
There are several common breast conditions that can affect people at any age. These include cysts, fibroadenomas (non-cancerous lumps), infections, and benign tumors. Most breast lumps are not cancerous, but any new lump should be checked by a healthcare provider.
Some people experience breast pain or tenderness, often related to their menstrual cycle or hormonal changes. Other possible changes include nipple discharge, redness, or swelling. Not all changes are linked to cancer, but monitoring for new symptoms is important.
Practicing breast self-awareness helps people notice changes early. Regular clinical breast exams and mammograms are also important tools for finding issues before they get worse. Breast health can also be influenced by injuries or diseases like diabetes, as explained at Crestwood Medical Center’s breast health page.
Risk Factors for Breast Disease
Certain factors raise the risk of developing breast cancer or other breast diseases. These include age (risk increases as one gets older), a family history of breast cancer, inherited gene mutations (such as BRCA1 or BRCA2), and having dense breast tissue.
Other risks include starting menstruation early, late menopause, use of hormone replacement therapy, and lifestyle choices like alcohol use or lack of physical activity. Having a personal history of breast cancer or some non-cancerous breast conditions can also make risk higher.
Understanding personal risk helps guide screening and prevention choices. Doctors may recommend more frequent screenings for people with higher risk. The Mayo Clinic’s guide to breast health gives more detail on who may be at greater risk and how to manage it.
Breast Cancer Overview
Breast cancer is one of the most common cancers in women and can appear in several forms. Understanding its main types, specific characteristics of lobular carcinoma, and prevention steps helps people make informed decisions about their health.
Types of Breast Cancer
There are several types of breast cancer, but the most common types include ductal carcinoma in situ (DCIS) and invasive ductal carcinoma (IDC). DCIS is a noninvasive form, meaning the cancer cells are only in the ducts and have not spread. IDC is the most common invasive type, where cancer cells break through the duct walls and spread to surrounding breast tissue.
Other less common types are inflammatory breast cancer, Paget’s disease of the breast, and triple-negative breast cancer. These forms can be more aggressive or require different treatments.
A comparison of main types:
| Type | Description |
|---|---|
| Ductal Carcinoma In Situ | Noninvasive, stays within breast ducts |
| Invasive Ductal Carcinoma | Spreads beyond ducts into other breast tissue |
| Lobular Carcinoma | Starts in lobules/glands that make milk |
Further reading is available at the Mayo Clinic’s guide to breast cancer types.
Lobular Carcinoma
Lobular carcinoma is a type of breast cancer that begins in the milk-producing glands, called lobules. There are two main forms: lobular carcinoma in situ (LCIS) and invasive lobular carcinoma (ILC).
LCIS is considered a marker for increased breast cancer risk but usually does not spread outside the lobules. ILC is more serious and can spread to surrounding tissues and, in some cases, to other parts of the body. This type of cancer may not form a lump and can be harder to detect during physical exams or on mammograms.
People might notice a thickening in the breast or changes in texture. Treatment depends on how far the cancer has spread. More details are available from the American Cancer Society’s overview.
Cancer Prevention
There are several practical steps people can take for cancer prevention related to breast health.
- Regular screening: Mammograms and clinical breast exams help find cancer early.
- Healthy lifestyle: Eating a balanced diet, staying active, and maintaining a healthy weight can reduce risk.
- Limiting alcohol: Alcohol increases breast cancer risk, so it is important to drink in moderation or not at all.
- Awareness of family history: Those with close relatives who have had breast cancer may need earlier or more frequent screenings.
Some women at higher risk may speak to their doctor about medicines or surgery to lower their chances. Good prevention strategies can lower risk but may not eliminate it completely. For more advice, visit the Cleveland Clinic’s breast cancer prevention tips.
Breast Health Screening and Early Detection
Screening helps doctors spot health problems in the breast before symptoms begin. Using reliable tests like mammograms can find cancer at an early stage and improve the chances for successful treatment.
Importance of Early Detection
Finding breast cancer early can make it easier to treat and can increase survival rates. Early detection usually means the cancer is found before it has spread. This can lead to less aggressive treatments and better recovery.
Some signs of breast cancer, such as lumps or changes in skin, are easier to treat when found early. Most early-stage breast cancers do not have symptoms, which is why regular screening is recommended, especially for women over 40.
Mammograms are the most effective screening tool for most women. Health organizations stress that regular mammograms can detect small tumors that may not be felt during a physical exam. Early detection lowers the risk of dying from breast cancer. More information can be found in this detailed guide on early detection and diagnosis.
Breast Cancer Screening Guidelines
Screening guidelines may change depending on a person’s age and risk level. Most experts recommend that women with average risk start yearly screening mammograms at age 40. Women with a higher risk, often due to family history or genetic factors, may need to start screening earlier or have extra tests like breast MRIs.
The American Cancer Society outlines when and how often to get screened. Regular mammograms are key, but some people may also need ultrasounds or doctor exams. It is important to speak with a healthcare provider to decide what schedule and tests are best. With proper screening, more cases are found in early stages, which can save lives. A simple table is shown below:
| Age Group | Suggested Screening |
|---|---|
| 40-44 | Optional yearly mammogram |
| 45-54 | Yearly mammogram |
| 55 and older | Mammogram every 1-2 years |
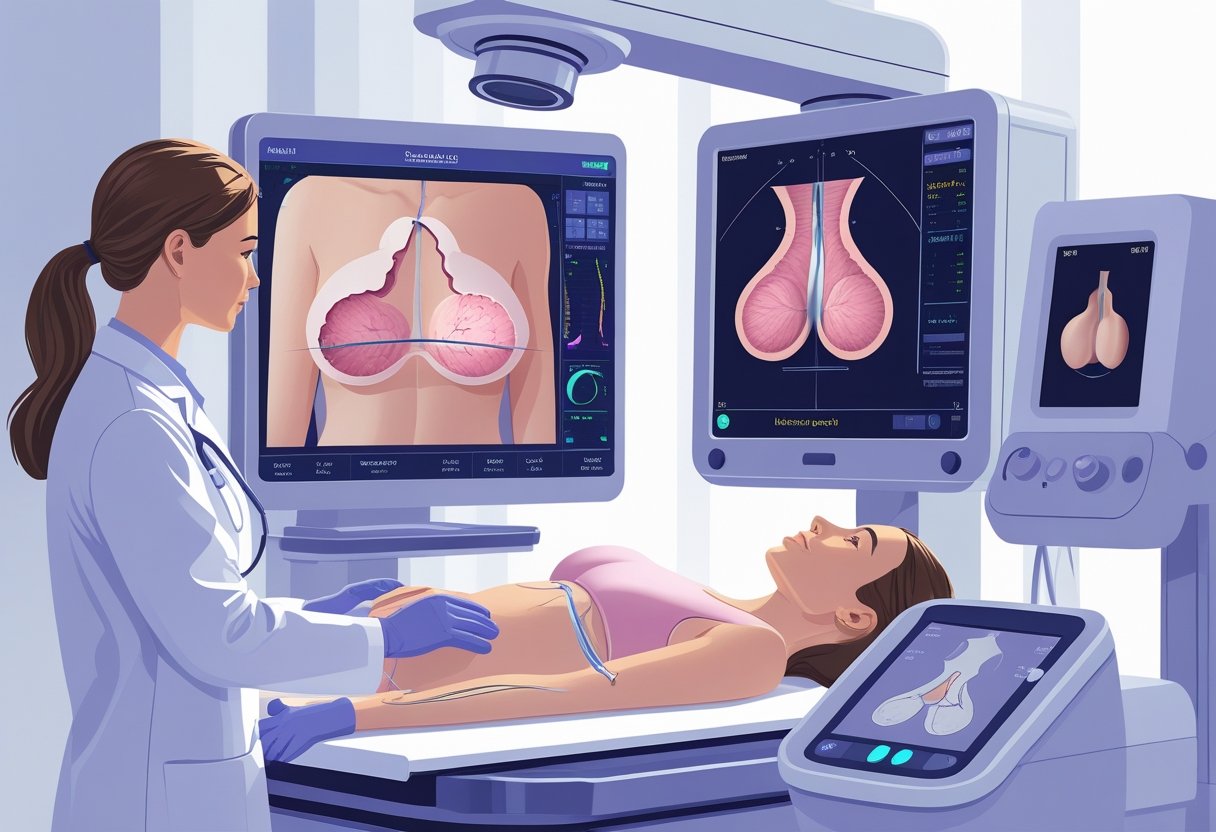
Diagnostic Tools and Procedures

Doctors use several methods to check for breast problems and diagnose breast cancer. These methods look for lumps, changes in breast tissue, or other signs that may need closer attention. Early detection is important because it can help with treatment options.
Clinical Breast Exam
A clinical breast exam is performed by a doctor or nurse. The healthcare provider carefully feels the breasts and underarm areas for lumps, changes in size, skin texture, or unusual thickening. This type of exam does not use machines or special equipment.
During the exam, the patient is usually seated and then lying down while the provider checks each breast. The provider may also ask questions about any pain, nipple discharge, or changes noticed at home.
If anything abnormal is found, the provider may suggest more tests like a mammogram or ultrasound. The clinical breast exam is often a routine part of a yearly physical for women.
Mammography
Mammography, or mammogram, is a special X-ray exam that takes detailed images of breast tissue. Radiologists review these images to look for small tumors or changes that are too tiny to feel by hand. The test can find signs of breast cancer early, often before symptoms appear.
There are two main types of mammograms: screening and diagnostic. Screening mammograms are done regularly for women who have no symptoms. Diagnostic mammograms are done if there is a symptom or a suspicious result from another test, like a lump or an abnormal screening.
The mammogram uses low-dose X-rays and usually takes about 20 minutes. The patient stands in front of the machine while each breast is placed on a flat plate and pressed gently. More details about this process are available on the Cleveland Clinic mammogram page.
Breast Ultrasound
A breast ultrasound uses sound waves to make images of the inside of the breast. This method does not use radiation. It is often used to help figure out if a breast lump is solid or filled with fluid.
Ultrasounds are done by moving a small handheld device, called a transducer, over the skin. The test is painless and usually takes about 15 to 30 minutes. Radiologists examine the images to see if there are cysts, lumps, or other changes.
Often, doctors use breast ultrasound alongside mammography or after an abnormal finding. It is especially useful for women with dense breast tissue since it can reveal things that may not show up as clearly on a mammogram. More information about this test can be found at Lahey Hospital's guide to diagnostic tools.
Advanced Imaging and Biopsy Techniques
Accurate imaging and precise tissue sampling help doctors detect breast cancer early and confirm a diagnosis. These methods can show tumors, help guide treatment, and reduce the chances of missing small or hard-to-find cancers.
Breast MRI
A breast MRI uses strong magnets and radio waves to take detailed pictures of the breast tissue. It does not use radiation like X-rays or CT scans. Breast MRIs are very helpful for women with dense breast tissue or high risk of breast cancer.
Doctors often use a breast MRI along with mammograms or ultrasounds to look for tumors that other tests may miss. This test is especially useful for pre-surgical planning and checking how well treatment is working. According to UCSF Health, breast MRI can help with the detection and diagnosis of breast cancer, particularly in challenging cases. Breast MRI may also use contrast, a special dye, to highlight abnormal areas.
Benefits of breast MRI:
- Finds small tumors not seen on mammograms
- Helps determine cancer stage
- Guides biopsies or surgery
Breast Biopsy
A breast biopsy is a procedure where a small piece of breast tissue is removed and checked for cancer cells by a pathologist. Several types of biopsies exist, including needle biopsies and surgical biopsies.
Most often, a needle biopsy is used because it is less invasive and can usually be done with local anesthesia. The doctor may use imaging tools, such as ultrasound or MRI, to guide the needle to the correct area. Pathologists then examine the tissue under a microscope to see if cancer or other diseases are present.
Examples of common breast biopsies include:
- Fine-needle aspiration
- Core needle biopsy
- Stereotactic biopsy
A breast biopsy helps confirm a diagnosis, which is needed to plan the right treatment.
Diagnosis and Staging of Breast Cancer
Breast cancer diagnosis relies on a mix of tests and doctors' teamwork. Early and accurate detection helps guide treatment and leads to better results for patients.
Breast Cancer Diagnosis Process
Doctors use several steps to diagnose breast cancer. The process usually starts with an imaging test like a mammogram or ultrasound if a lump or changes in the breast are found. If anything looks unusual, a biopsy may be done. This involves removing a small sample of tissue so a pathologist can check for cancer cells.
After cancer is found, other tests help figure out the stage of the disease. Staging means finding out how large the tumor is, whether cancer has spread to nearby lymph nodes, or if it has traveled to other parts of the body. Doctors use imaging studies and sometimes blood tests for staging.
The stages of breast cancer range from stage 0, which is very early, to stage 4, where cancer has spread further. Lower stages are usually less advanced and have better outcomes. To learn more, visit this stages of breast cancer page.
Role of Multidisciplinary Teams
Breast cancer care often involves a team of doctors. These teams include oncologists, who focus on cancer treatment, breast surgeons, who perform surgery, and sometimes nurses, radiologists, and counselors. Each expert plays a key role during diagnosis and treatment.
The team meets to discuss each patient’s test results and work out a treatment plan that fits the cancer's stage and type. This approach helps make sure that all options are considered for the best patient care and outcomes.
Collaboration between specialists means that decisions are based on both the specifics of the cancer and the person’s individual needs. This teamwork is now the standard of care for breast cancer at most large hospitals and cancer centers.
Treatment Strategies and Options
Breast cancer treatment often involves a combination of medical procedures and targeted therapies. Choices vary based on the cancer stage, tumor type, and patient health.
Surgical Options
Surgery is usually the first step in breast cancer treatment. It can involve the removal of just the tumor (lumpectomy) or the entire breast (mastectomy). The selection depends on tumor size, location, and personal preferences.
In some cases, lymph nodes near the breast are also removed and checked for cancer. This helps the doctor decide if more treatment is needed. Surgical treatment options are tailored to provide the best chances of removing cancer while trying to save as much healthy tissue as possible.
Recovery from surgery can include pain, swelling, or changes in breast shape. Doctors may suggest reconstructive surgery to rebuild the breast’s appearance. For more details about surgical treatments, see the comprehensive overview on breast cancer surgical options.
Radiation and Medical Therapies
Radiation therapy uses high-energy rays to kill cancer cells that might remain after surgery. It is often given after a lumpectomy and sometimes after a mastectomy when there is a higher risk the cancer could come back.
Medical treatments for breast cancer include chemotherapy, hormone therapy, and targeted therapy. Chemotherapy uses medicines to kill cancer cells throughout the body. Hormone therapy blocks hormones that fuel the growth of certain cancers. Targeted therapies focus on specific parts of cancer cells to stop their growth.
Doctors choose these treatment strategies based on the cancer’s characteristics and the patient’s overall health. You can learn more about these approaches to breast cancer treatment from the American Cancer Society’s treatment options and the CDC’s breast cancer care page.
Recovery and Support After Treatment
After breast cancer treatment, most people go through a stage of recovery and need regular support. Services and follow-up appointments help address physical changes, emotional health, and long-term well-being.
Post-Treatment Recovery
Recovery after treatment can be challenging. Patients often deal with tiredness, body changes, or side effects from surgery, chemotherapy, or radiation.
Many hospitals and clinics offer special breast health services that focus on rehabilitation. These services might include physical therapy, pain management, counseling, and nutrition advice. Some programs, like the Recovery Package, help patients regain strength and adjust to life after cancer by offering structured care, support, and health checks. Learn more about the Recovery Package and ongoing support.
It's also important for patients to practice self-care, such as eating a healthy diet, getting exercise, and finding emotional support. Support groups or therapy can help with stress, sadness, or anxiety that sometimes happen after treatment. Find tips for lifestyle changes after breast cancer.
Follow-Up Care
After treatment, most people have regular follow-up visits with their medical team. These check-ups monitor for any signs that the cancer has come back and look for new health problems.
Common parts of follow-up care include:
- Breast exams and imaging
- Checking for side effects from past treatments
- Managing other health conditions
Doctors may also create a survivorship care plan that lists future appointments, recommended tests, and suggestions for staying healthy. Keeping a record of all treatments and appointments is helpful to track progress and plan ahead. Details about follow-up care after breast cancer treatment can help patients know what to expect.
Research, Innovation, and Quality Standards
Breast health care has advanced through focused medical research and strong quality measures. New treatments, better imaging, and careful oversight help improve care for patients with breast conditions.
Clinical Trials in Breast Cancer
Clinical trials have brought new ways to detect and treat breast cancer. Researchers test medicine, therapy, and new technology on groups of people in well-planned studies. Patients join these trials for new treatments, sometimes before they are widely available.
Major trials are conducted by hospitals, cancer centers, and government groups like the National Cancer Institute. These studies check both how well treatments work and how safe they are. Clinical trials collect valuable data on side effects, recovery, and survival.
Anyone thinking of joining a trial should speak with their doctor. Participation can give access to advanced care while helping improve care for others in the future.
Centers of Excellence
A Center of Excellence is a hospital or clinic with the highest level of expertise in breast health. These centers provide care by teams of specialized doctors, nurses, and support staff. Facilities like these offer advanced treatments, genetic testing, and support programs.
Many centers are approved by the National Cancer Institute or the Commission on Cancer. They follow strict guidelines for quality and patient safety. Patients often get access to the latest research studies and clinical trials.
Centers of Excellence also provide second opinions and coordinate care with other doctors. Their strong teamwork helps patients get better treatment and support at every step.
Quality and Accreditation
Quality and safety are important in breast care. There are strong quality standards for breast imaging and screening that hospitals must meet. The Mammography Quality Standards Act (MQSA) is a federal law that sets standards for mammogram facilities. The U.S. Food and Drug Administration (FDA) checks that clinics follow these rules, including reporting breast density and having regular inspections.
Accreditation is given by groups such as the American College of Radiology. It means a facility meets strict standards on staff qualifications, equipment, and care. Patients should look for accredited centers to make sure they get the best quality of care. Regular reviews keep standards high and protect patient safety.
Below is a simple comparison:
| Standard | Who Sets It | What It Covers |
|---|---|---|
| MQSA | U.S. FDA | Mammography quality, safety |
| ACR Accreditation | American College of Radiology | Equipment, staff, procedures |
| NCI Designation | National Cancer Institute | Advanced research, patient care |
Frequently Asked Questions
Taking care of breast health includes eating well, staying active, checking for changes, and understanding early warning signs. Making smart choices and paying attention can make a difference.
What dietary choices can support optimal breast health?
Eating more fruits and vegetables like berries, leafy greens, and broccoli can benefit breast health. Choosing whole grains, beans, and lean proteins such as fish or chicken is also helpful. Reducing processed foods, sugary drinks, and alcohol is recommended to help lower risk, as a healthy diet can help prevent breast cancer.
Which exercises are recommended for maintaining healthy breasts?
Regular physical activity such as brisk walking, swimming, and cycling supports healthy breasts. Strength training like lifting light weights also helps by keeping the body fit and managing weight. Aim for at least 150 minutes of moderate exercise each week.
How can early breast cancer detection be effectively practiced at home?
A monthly self-exam helps people notice any unusual lumps or changes. Doing the exam at the same time each month, such as a few days after a period, can make it easier to detect changes. If someone feels or sees anything unusual, they should contact a doctor soon.
What are the early signs and symptoms to look out for in breast health?
Watch for lumps, swelling, pain, skin dimpling, or unusual changes in the breast or nipple. Notice any nipple discharge other than breast milk. Early detection is important, so report any signs to a healthcare provider quickly. Read more about first signs of breast cancer.
What lifestyle modifications can reduce the risk of breast cancer?
Not smoking, limiting alcohol, eating a balanced diet, staying active, and maintaining a healthy weight all lower risk. Managing stress and getting enough sleep also help. Some of these changes are shown to reduce breast cancer risk.
How often should one perform self-examinations for breast health?
Most experts suggest doing a breast self-exam once a month. This routine can help a person learn what is normal and notice changes earlier. If someone is not sure how to perform a self-exam, a healthcare professional can teach the correct steps.

