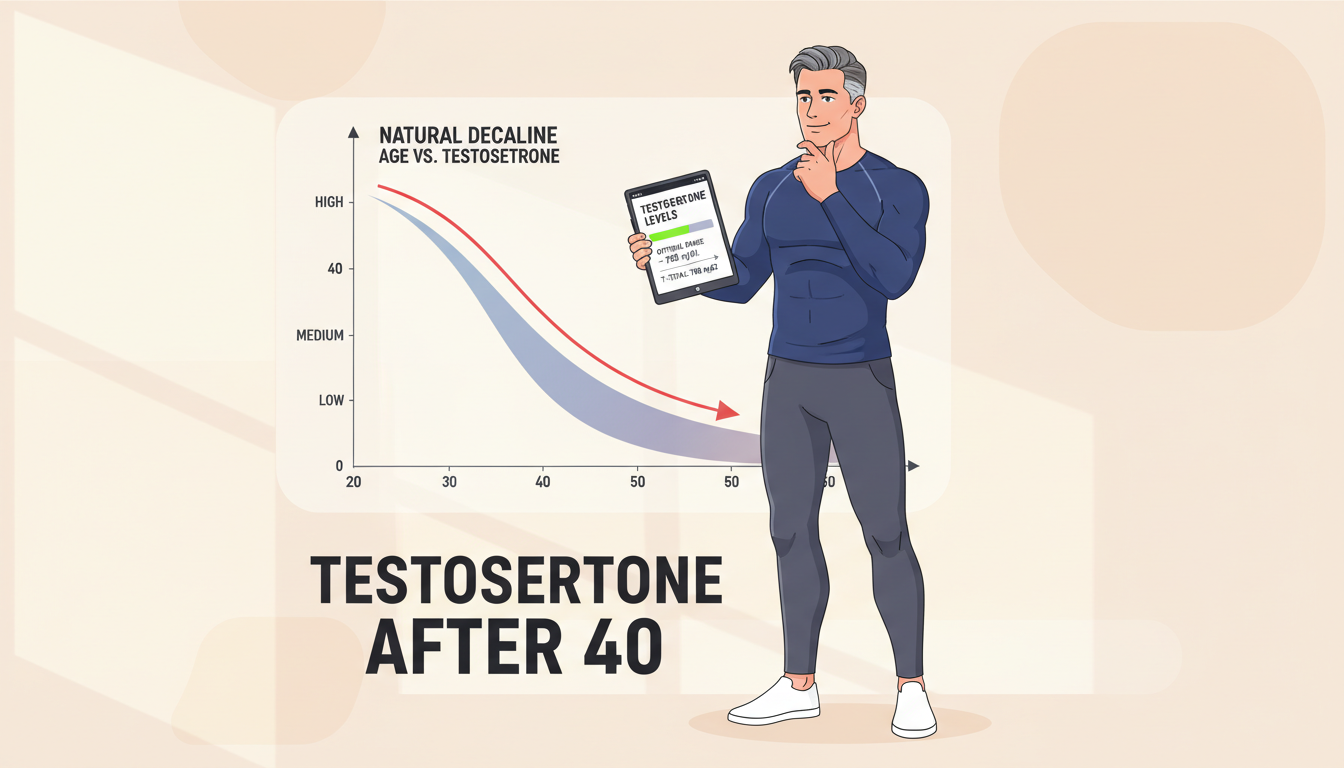
Reaching the age of forty marks a pivotal juncture in masculine vitality. Your body begins a subtle yet profound metamorphosis as testosterone levels commence their gradual descent. This androgenic hormone, responsible for muscle density, libido, energy reserves, and mental acuity, diminishes at approximately 1-2% annually after crossing this threshold. The ramifications extend beyond physical manifestations—affecting mood regulation, metabolic efficiency, and overall quality of existence. Understanding testosterone after 40 empowers men to reclaim their vigor through evidence-based interventions that support hormonal equilibrium naturally.
The Science Behind Testosterone Decline After Age 40
What Happens to Hormones After Forty
The hypothalamic-pituitary-testicular axis undergoes significant alterations as men surpass thirty-five years. Total serum testosterone decreases at 0.4% yearly, while free testosterone—the bioavailable form—plummets at a steeper 1.3% per annum in males aged 40-70. This dual decline creates a compounding effect on masculine health markers.
Over a third of men beyond forty-five exhibit testosterone concentrations below age-appropriate thresholds. The pituitary gland’s responsiveness to gonadotropin-releasing hormone weakens, resulting in diminished luteinizing hormone secretion that signals testosterone production.
Cellular Changes in the Testes
Leydig cells, the testosterone-producing workhorses within testicular tissue, lose their responsiveness to hormonal signals. Chronic inflammation becomes a hallmark of aging tissue, with activated macrophages releasing reactive oxygen species that suppress testosterone synthesis. This inflammatory milieu creates a hostile environment for optimal androgen production.
Additionally, endoplasmic reticulum stress increases within aging cells, triggering apoptotic pathways that further compromise testosterone manufacturing capacity. These microscopic changes accumulate into measurable hormonal deficits.
Why Free Testosterone Matters Most
Free testosterone represents the unbound, biologically active fraction circulating in your bloodstream. Sex hormone-binding globulin increases with age, sequestering more testosterone in an inactive state. This explains why men may experience low testosterone symptoms despite seemingly normal total testosterone measurements.
The accelerated decline of free testosterone at 1.3% annually compounds physical and cognitive deterioration more rapidly than total testosterone reductions. Monitoring both metrics provides comprehensive insight into hormonal status.
Recognizing the Symptoms of Low Testosterone After 40
Physical Manifestations You Cannot Ignore
Muscle mass atrophy occurs insidiously as testosterone levels wane. Sarcopenia—age-related muscle loss—accelerates when androgen concentrations fall below optimal ranges. Bone mineral density decreases simultaneously, elevating fracture susceptibility.
Visceral adiposity accumulates preferentially around the midsection. This creates a vicious cycle, as adipose tissue harbors aromatase enzymes that convert testosterone into estrogen. Facial and body hair thinning represents another visible indicator of declining androgens.
Mental and Emotional Red Flags
Depression, irritability, and cognitive fog frequently accompany testosterone deficiency. Motivation diminishes, and the zest for previously enjoyable activities evaporates. These neuropsychiatric symptoms often get misattributed to stress or aging alone.
Concentration difficulties and memory lapses intensify as testosterone receptors in the hippocampus receive insufficient hormonal signaling. The brain requires adequate androgens for optimal neurotransmitter function and neuroplasticity maintenance.
Sexual Health Indicators
Libido reduction represents the most recognized symptom of testosterone after 40 decline. Erectile quality deteriorates as nitric oxide production decreases and vascular smooth muscle responsiveness declines. Morning erections become less frequent or disappear entirely.
Diminished sexual satisfaction affects relationship dynamics and self-perception. These intimacy challenges often motivate men to finally seek hormonal evaluation after ignoring other warning signs.
Fix Number One: Strategic Resistance Training Protocols
The Anabolic Response to Heavy Lifting
Resistance exercise stimulates acute testosterone elevation lasting 15-60 minutes post-workout. More importantly, consistent strength training enhances receptor sensitivity, allowing existing testosterone to function more effectively. This dual mechanism amplifies hormonal benefits without pharmaceutical intervention.
Lifting loads between 85-95% of your one-repetition maximum generates the most robust anabolic response. Compound movements engaging multiple muscle groups—squats, deadlifts, bench presses, rows—trigger greater hormonal cascades than isolation exercises.
Frequency and Volume Considerations
Training three days weekly for four weeks produces measurable testosterone increases both acutely and chronically. Greater volume and intensity correlate with amplified hormonal responses. However, overtraining induces cortisol elevation that counteracts testosterone production.
Optimal protocols balance mechanical tension with adequate recovery intervals. Sessions lasting 45-60 minutes maximize anabolic signaling without triggering excessive catabolic stress.
High-Intensity Interval Training Benefits
HIIT workouts complement resistance training by boosting testosterone through metabolic stress pathways. These brief, intense efforts stimulate growth hormone release alongside testosterone, creating synergistic anabolic effects. Sprint intervals, battle ropes, and kettlebell circuits exemplify effective modalities.
Endurance-based cardio, conversely, may reduce testosterone concentrations when performed excessively. Moderate cardiovascular exercise supports overall health without hormonal suppression, making strategic programming essential.

Fix Number Two: Nutritional Optimization for Hormonal Health
Micronutrients Essential for Testosterone Synthesis
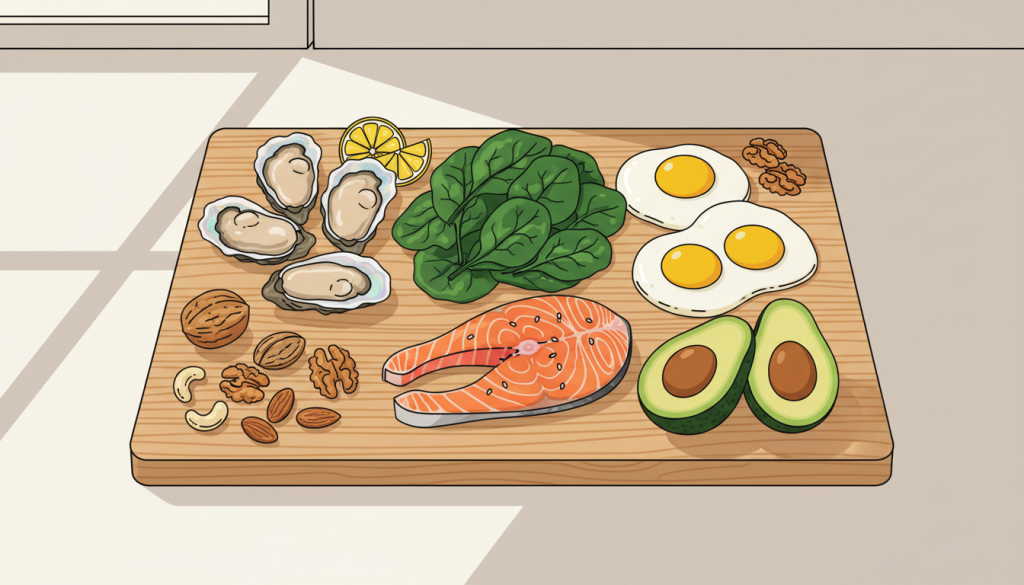
Zinc deficiency directly correlates with suppressed testosterone concentrations. This mineral serves as a cofactor for enzymes catalyzing androgen production within Leydig cells. Supplementation in marginally deficient men restores serum testosterone to normal ranges.
Oysters contain the highest zinc concentrations of any food, followed by beef, pumpkin seeds, and cashews. Consuming two Brazil nuts daily provides selenium, another crucial mineral for testicular function.
Vitamin D’s Hormonal Influence
Vitamin D functions as a steroid hormone precursor, directly regulating testosterone synthesis. Individuals with insufficient cholecalciferol levels demonstrate lower androgen concentrations. Sun exposure remains the optimal source, though fatty fish like salmon, egg yolks, and fortified dairy provide dietary alternatives.
Many men require supplementation even with regular sunlight exposure, particularly those residing in northern latitudes. Testing vitamin D status guides appropriate supplementation dosing.
Healthy Fats for Hormone Production
Testosterone synthesis requires cholesterol as the molecular backbone. Diets excessively low in dietary fats compromise hormonal production. Olive oil, avocados, nuts, and fatty fish supply monounsaturated and omega-3 fatty acids that support endocrine function without inflammatory consequences.
Trans fats and excessive refined vegetable oils promote oxidative stress and insulin resistance, indirectly suppressing testosterone. Emphasizing whole food fat sources optimizes hormonal substrates.
Foods That Sabotage Testosterone
Excess alcohol consumption disrupts the hypothalamic-pituitary-testicular axis and directly damages Leydig cells. Refined sugars spike insulin, triggering aromatase activity that converts testosterone to estrogen. Phytoestrogens in excessive soy intake may compete with androgen receptors, though moderate consumption appears benign.
Certain dairy products contain bovine hormones that potentially interfere with human endocrine signaling. Selecting organic, grass-fed dairy mitigates this concern.
Strategic Meal Timing
Intermittent fasting protocols may enhance insulin sensitivity and growth hormone secretion, indirectly supporting testosterone. However, chronic caloric restriction elevates cortisol and suppresses reproductive hormones. Balanced meal timing with adequate protein distribution sustains anabolic conditions.
Pre-workout nutrition fuels training intensity that stimulates hormonal responses. Post-workout nutrition capitalizes on the anabolic window when testosterone receptors demonstrate heightened sensitivity.
Fix Number Three: Sleep Architecture and Circadian Optimization
Testosterone’s Nocturnal Production Cycle
The majority of daily testosterone production occurs during deep sleep stages. Levels typically peak around 8 AM and nadir around 8 PM, following a circadian rhythm facilitated by quality slumber. This oscillating pattern maintains hormonal homeostasis and receptor sensitivity.
Sleep restriction to five hours nightly for one week decreased daytime testosterone by 10-15% in healthy young males. The cumulative effect of chronic sleep deprivation accelerates age-related testosterone decline.
Sleep Quality Versus Quantity
Seven to eight hours represents the minimum threshold for optimal testosterone production. However, duration alone proves insufficient—sleep architecture quality determines hormonal output. Frequent awakenings and inability to reach slow-wave sleep disrupt the natural testosterone release cycle.
REM sleep and deep sleep stages demonstrate the highest androgenic hormone secretion. Sleep fragmentation prevents adequate time in these restorative phases.
Sleep Apnea’s Devastating Effects
Obstructive sleep apnea causes repeated nocturnal awakenings that jolt the body from deep sleep. Hypoxemia—reduced blood oxygen—during apneic episodes triggers oxidative stress that damages testicular tissue. Men with untreated sleep apnea demonstrate markedly suppressed testosterone concentrations.
CPAP therapy normalizes sleep architecture and frequently restores testosterone levels without additional intervention. Screening for sleep-disordered breathing should accompany testosterone evaluations.
Circadian Rhythm Entrainment Strategies
Morning sunlight exposure synchronizes the suprachiasmatic nucleus, strengthening circadian amplitude. This enhances the differentiation between peak morning testosterone and evening nadir. Blue light blocking in the evening supports melatonin secretion that facilitates sleep onset.
Consistent sleep-wake schedules, even on weekends, reinforce circadian rhythms. Temperature regulation—cooler bedroom environments around 65-68°F—promotes deeper sleep stages conducive to testosterone production.
Stress Reduction and Cortisol Management
Chronic psychological stress elevates cortisol, the catabolic hormone that directly antagonizes testosterone. The hypothalamic-pituitary-adrenal axis, when persistently activated, suppresses the hypothalamic-pituitary-testicular axis. This creates a hormonal seesaw where stress hormone predominance diminishes reproductive hormones.
Mindfulness practices, adequate sleep, and regular exercise mitigate stress physiology. Adaptogenic herbs like ashwagandha may buffer cortisol responses, though individual responses vary.

Body Composition Changes and Testosterone Interactions
The Adiposity-Androgen Vicious Cycle
Excess body fat, particularly visceral adiposity, harbors aromatase enzymes converting testosterone into estradiol. This biochemical transformation depletes circulating androgens while elevating estrogen concentrations. The resulting hormonal imbalance further promotes fat accumulation and muscle catabolism.
Obesity and testosterone deficiency mutually exacerbate each other. Treating low testosterone improves insulin sensitivity, facilitates fat oxidation, and enhances metabolic health. Concurrent lifestyle modifications amplify these beneficial effects.
Muscle Mass as Metabolic Currency
Skeletal muscle tissue functions as an endocrine organ secreting myokines that influence systemic metabolism. Greater muscle mass improves glucose disposal, reduces inflammation, and supports favorable hormonal profiles. The anabolic effects of testosterone manifest primarily through enhanced protein synthesis in muscle tissue.
Preserving lean body mass becomes paramount after forty when sarcopenia accelerates. Resistance training combined with adequate protein intake counteracts age-related muscle atrophy.
Metabolic Syndrome and Hormonal Health
Insulin resistance, hypertension, dyslipidemia, and central obesity comprise metabolic syndrome—a constellation of conditions associated with low testosterone. Hyperinsulinemia suppresses sex hormone-binding globulin production, paradoxically increasing free estrogen while reducing free testosterone. Addressing metabolic dysfunction often normalizes hormonal parameters without direct intervention.
Lifestyle modifications targeting metabolic health synergistically improve testosterone concentrations. This approach addresses root pathophysiology rather than merely symptom management.
Understanding Testosterone Replacement Therapy Options
When Pharmaceutical Intervention Becomes Necessary
Testosterone replacement therapy (TRT) suits men with clinically diagnosed hypogonadism—persistent symptoms coupled with confirmed low testosterone measurements. Trials should only commence after exhausting lifestyle optimization strategies. Appropriate patient selection minimizes risks while maximizing therapeutic benefits.
TRT improves libido, sexual function, bone mineral density, muscle mass, and body composition in hypogonadal men. These benefits must be weighed against potential adverse effects including polycythemia, sleep apnea exacerbation, and fertility suppression.
TRT Delivery Modalities Explained
Intramuscular injections, transdermal gels, subcutaneous pellets, and buccal tablets represent available delivery systems. Each modality demonstrates unique pharmacokinetic profiles affecting dosing frequency and serum concentration stability. Injections provide cost-effectiveness but create peak-trough fluctuations.
Transdermal preparations maintain steadier levels but risk transfer to intimate contacts. Patient preference, lifestyle factors, and physiological response guide modality selection.
Monitoring and Risk Mitigation
Men receiving TRT require surveillance for polycythemia—excessive red blood cell production that increases thrombotic risk. Hematocrit monitoring every 3-6 months identifies this complication early. Prostate-specific antigen tracking remains controversial, as TRT does not cause prostate cancer but may accelerate existing malignancies.
Exogenous testosterone suppresses gonadotropin release, inducing testicular atrophy and azoospermia. Men desiring future fertility should avoid TRT or consider alternatives like clomiphene citrate that preserve spermatogenesis.
Realistic Expectations and Timeline
Therapeutic effects manifest gradually over weeks to months. Libido improvements often appear within 3-6 weeks, while body composition changes require 12-16 weeks. Energy enhancement and mood stabilization demonstrate variable timelines among individuals.
TRT represents a long-term commitment requiring consistent administration and medical monitoring. Abrupt discontinuation causes testosterone levels to plummet below pre-treatment baselines temporarily.
The Psychological Dimensions of Hormonal Change
Mood Regulation and Emotional Stability
Testosterone receptors densely populate limbic system structures governing emotional processing. Inadequate androgen signaling correlates with depression, anxiety, and irritability. The neurobiological mechanisms involve neurotransmitter modulation—particularly dopamine, serotonin, and GABA systems.
Addressing testosterone deficiency often alleviates psychiatric symptoms resistant to conventional antidepressant therapy. However, hormonal optimization complements rather than replaces comprehensive mental health treatment.
Cognitive Function and Neuroplasticity
Spatial cognition, working memory, and processing speed demonstrate testosterone-dependent elements. Hippocampal neurogenesis—the birth of new neurons—requires adequate androgen concentrations. Age-related cognitive decline accelerates when testosterone levels fall below threshold concentrations.
Maintaining optimal testosterone through midlife may preserve cognitive reserve and delay neurodegenerative processes. This neuroprotective hypothesis requires further longitudinal validation.
Motivation and Drive Restoration
Androgens influence reward circuitry and goal-directed behavior through dopaminergic pathways. Diminished testosterone manifests as apathy, reduced competitive drive, and decreased ambition. Men describe feeling like shadows of their former selves when hormones decline significantly.
Restoring testosterone often reignites purposeful engagement with life pursuits. This psychological rejuvenation extends beyond physical improvements alone.
Cardiovascular Health Considerations
The Testosterone-Heart Disease Debate
Historical concerns about TRT increasing cardiovascular risk have been challenged by more rigorous recent studies. Men with low testosterone actually demonstrate higher cardiovascular mortality and morbidity. Physiological testosterone concentrations appear cardioprotective through multiple mechanisms.
Adequate androgens improve endothelial function, reduce visceral adiposity, enhance insulin sensitivity, and favorably modify lipid profiles. These metabolic improvements translate to reduced atherosclerotic risk.
Blood Pressure and Vascular Function
Testosterone influences nitric oxide bioavailability—the primary vasodilator mediating blood pressure regulation. Some men experience blood pressure elevations on TRT, while others demonstrate improvements. Individual cardiovascular response profiles necessitate personalized monitoring.
Resistance training combined with testosterone optimization enhances arterial compliance and reduces peripheral vascular resistance. Synergistic lifestyle factors amplify cardiovascular benefits.
Lipid Profile Implications
TRT typically reduces HDL cholesterol modestly while variably affecting LDL and triglycerides. The clinical significance of HDL reduction remains uncertain, as other cardiovascular risk markers often improve. Comprehensive risk assessment rather than isolated lipid values guides cardiovascular management.
Dietary interventions emphasizing monounsaturated fats and omega-3 fatty acids may offset unfavorable lipid shifts associated with testosterone therapy.

Advanced Lifestyle Factors Influencing Testosterone
Environmental Endocrine Disruptors
Xenoestrogens—synthetic compounds with estrogen-like activity—pervade modern environments. Bisphenol-A in plastics, phthalates in personal care products, and pesticide residues in conventional produce disrupt endocrine signaling. These chemicals competitively bind androgen receptors or enhance aromatase activity.
Minimizing exposure through glass storage containers, organic produce selection, and natural personal care products reduces xenoestrogen burden. Water filtration removes numerous endocrine-disrupting contaminants.
Alcohol Consumption Patterns
Moderate alcohol intake—defined as 1-2 drinks daily—demonstrates neutral to slightly negative effects on testosterone. Heavy episodic drinking and chronic excessive consumption directly damage Leydig cells and disrupt the hypothalamic-pituitary axis. Alcoholic beverages also contribute empty calories that promote adiposity.
Complete abstinence may not be necessary for hormonal health, but limiting consumption to occasional moderate intake optimizes endocrine function. Individual tolerance varies based on genetic alcohol metabolism capacity.
Thermal Stress on Testicular Function
Testicular tissue resides in the scrotum because optimal spermatogenesis and testosterone production require temperatures 2-4°C below core body temperature. Frequent hot tub use, laptop heat exposure, and tight undergarments elevate scrotal temperature sufficiently to impair Leydig cell function.
Boxers versus briefs debates hold physiological merit. Avoiding prolonged heat exposure to the genital region preserves testicular microenvironment homeostasis.
Supplement Science: What Works and What Wastes Money
Evidence-Based Nutraceuticals
Vitamin D supplementation corrects deficiency states that suppress testosterone. Zinc supplementation benefits men with inadequate dietary intake or marginal deficiency. Magnesium demonstrates modest benefits, particularly in physically active individuals. These foundational micronutrients address nutritional insufficiencies rather than pharmacologically boosting hormones supraphysiologically.
D-aspartic acid, fenugreek extract, and Tribulus terrestris lack consistent evidence supporting testosterone elevation in non-deficient men. Marketing claims frequently exceed scientific substantiation.
Ashwagandha and Adaptogenic Herbs
This Ayurvedic botanical demonstrates stress-buffering properties that indirectly support testosterone by mitigating cortisol excess. Several studies show modest testosterone increases in stressed individuals supplementing with standardized ashwagandha extracts. The mechanism likely involves hypothalamic-pituitary axis modulation rather than direct testicular stimulation.
Quality and standardization vary dramatically among ashwagandha products. Selecting reputable brands with third-party testing ensures active constituent concentrations.
The Creatine Connection
Creatine monohydrate supplementation enhances resistance training performance and muscle hypertrophy. Some research suggests creatine may influence dihydrotestosterone—a more potent androgen metabolite. However, evidence remains insufficient to recommend creatine specifically for testosterone enhancement versus its well-established ergogenic benefits.
Five grams daily represents standard effective dosing. Loading phases offer no long-term advantage over consistent maintenance dosing.
Avoiding Proprietary Blend Pitfalls
Testosterone boosters containing proprietary blends obscure individual ingredient dosages, preventing efficacy assessment. Many formulations include under-dosed ingredients combined with stimulants that create subjective energy perception without hormonal changes. Transparency in labeling indicates manufacturer confidence and allows scientific evaluation.
Single-ingredient supplements targeting verified nutritional deficiencies provide superior value compared to kitchen-sink formulations making exaggerated claims.
Social and Relationship Impacts
Intimacy and Partnership Dynamics
Declining libido and erectile difficulties strain romantic relationships when partners misinterpret symptoms as disinterest or attraction loss. Open communication about hormonal changes prevents misunderstandings and fosters collaborative problem-solving. Many couples report relationship improvements following testosterone optimization.
Partners may notice mood improvements, increased initiative, and restored vitality before the man himself recognizes changes. External perspectives validate treatment efficacy.
Social Confidence and Professional Performance
Testosterone influences dominance behaviors, risk tolerance, and competitive drive—traits affecting professional success in certain contexts. Men with optimized hormones report enhanced workplace confidence, negotiation assertiveness, and leadership presence. These subjective improvements reflect neurobiological changes in limbic and prefrontal circuits.
The societal stigma surrounding male hormonal health prevents many men from seeking evaluation until symptoms become severe. Normalizing discussions about testosterone after 40 facilitates earlier intervention.
Physical Appearance and Self-Perception
Muscle definition, facial structure, and body composition influence self-image and social perception. Testosterone’s anabolic effects enhance physical markers associated with vitality and attractiveness. These changes extend beyond vanity, affecting psychological well-being and social interactions.
Improved physical capacity enables recreational activities and hobbies that enrich life quality. The indirect benefits of hormonal optimization radiate throughout multiple life domains.
Medical Testing and Diagnosis Protocols
When to Request Testosterone Screening
Men experiencing multiple symptoms—fatigue, reduced libido, mood changes, strength decline—warrant hormonal evaluation regardless of age. However, isolated nonspecific symptoms require comprehensive assessment excluding other causes before attributing them to testosterone deficiency. Thyroid disorders, anemia, depression, and sleep apnea mimic hypogonadism.
Morning blood draws between 7-11 AM capture peak testosterone concentrations, providing standardized measurement conditions. Single measurements may not reflect true status due to daily fluctuations and episodic secretion patterns.
Understanding Laboratory Results
Total testosterone below 300 ng/dL generally indicates hypogonadism, while levels above 1000 ng/dL represent the upper normal range. However, symptoms correlate better with free testosterone concentrations. Reference ranges reflect population distributions rather than optimal individual values.
Some men experience symptoms at 400 ng/dL while others remain asymptomatic at 250 ng/dL. Clinical context trumps arbitrary numerical thresholds when making treatment decisions.
Additional Hormonal Parameters
Luteinizing hormone and follicle-stimulating hormone levels distinguish primary testicular failure from secondary hypothalamic-pituitary dysfunction. Prolactin elevation suppresses gonadotropin secretion, causing secondary hypogonadism. Estradiol measurement identifies excessive aromatization.
Comprehensive panels guide diagnosis accuracy and inform treatment selection. Sex hormone-binding globulin calculation enables free testosterone estimation when direct measurement proves unavailable.
Repeat Testing and Confirmation
A single low measurement requires confirmation through repeat testing before initiating lifelong therapy. Transient factors—illness, stress, insufficient sleep—temporarily suppress testosterone. Confirming persistent deficiency prevents unnecessary treatment in men with situational fluctuations.
Testing both total and free testosterone on at least two separate occasions establishes reliable diagnosis. Morning collection timing remains essential for standardization.

Realistic Timeline for Natural Interventions
First Month Expectations
Implementing sleep optimization, resistance training, and dietary improvements initiates hormonal shifts within weeks. Subjective energy improvements often precede measurable testosterone changes. Sleep quality enhancements manifest most rapidly, followed by training adaptations.
Consistency determines success more than perfection. Establishing sustainable routines proves more valuable than unsustainable extreme measures attempted briefly.
Three-Month Assessment Window
Significant body composition changes—increased lean mass, reduced body fat—typically require 8-12 weeks of consistent intervention. Testosterone level improvements plateau after several months of lifestyle optimization. This timeframe allows realistic efficacy evaluation before considering pharmaceutical options.
Patience remains essential, as hormonal systems respond gradually to sustained behavioral changes. Frequent testing during this period proves unnecessary and potentially discouraging.
Long-Term Maintenance Strategies
Sustaining testosterone after 40 requires ongoing commitment to health practices rather than temporary fixes. Aging continues regardless of interventions, necessitating adaptation of training intensity, nutritional needs, and recovery protocols over time. Annual or biannual testing monitors hormonal trajectory and informs strategy adjustments.
Viewing testosterone optimization as lifelong health investment rather than short-term project fosters adherence and maximizes cumulative benefits over decades.
Debunking Common Testosterone Myths
The Aggression Misconception
Media portrayals equate testosterone with uncontrolled aggression and reckless behavior. Research contradicts this oversimplification—adequate testosterone actually improves mood stability and reduces irritability associated with deficiency. Supraphysiological doses used in anabolic steroid abuse differ fundamentally from optimization therapy.
Contextual factors and personality traits exert greater influence on aggressive behavior than hormonal concentrations within normal ranges. Testosterone modulates rather than determines behavioral expression.
The Prostate Cancer Controversy
Historical belief that testosterone causes prostate cancer persists despite lack of supporting evidence. Low testosterone correlates with more aggressive prostate malignancies when they occur. TRT does not increase prostate cancer incidence but may accelerate pre-existing occult tumors.
Appropriate screening before and during therapy mitigates risks. The testosterone-prostate relationship proves more nuanced than simplistic cause-effect models suggest.
The Permanent Dependency Fear
Men worry that initiating TRT creates lifelong pharmaceutical dependence. While exogenous testosterone suppresses endogenous production during treatment, discontinuation allows natural production to resume in most cases. Recovery timelines vary, with younger men demonstrating faster rebound.
However, if underlying age-related decline prompted treatment, stopping therapy typically returns testosterone to pre-treatment levels. This represents restoration to baseline rather than induced deficiency.
Comparing Natural Optimization Versus TRT
Efficacy Magnitude Differences
Lifestyle interventions may increase testosterone by 100-300 ng/dL in men with modifiable risk factors—meaningful improvements addressing mild to moderate deficiency. TRT elevates levels to mid-normal or upper-normal ranges regardless of baseline, typically increasing concentrations by 300-500 ng/dL or more.
Men with profound hypogonadism—levels below 200 ng/dL—benefit most from pharmaceutical intervention, while those with borderline levels often respond adequately to lifestyle modifications alone.
Risk-Benefit Considerations
Natural approaches carry virtually no adverse effects when implemented sensibly, offering additional health benefits beyond testosterone elevation. TRT introduces potential complications requiring medical monitoring and informed consent. Individual risk tolerance and symptom severity guide decision-making.
Many men achieve satisfaction through lifestyle optimization, avoiding pharmaceutical costs and surveillance requirements. Others require TRT for adequate symptom resolution and quality-of-life restoration.
Cost and Accessibility Factors
Resistance training, sleep improvement, and dietary modifications require time investment and potential gym membership costs but avoid ongoing pharmaceutical expenses. TRT involves medication costs, laboratory monitoring expenses, and clinical visit copays. Insurance coverage varies, with some plans restricting access through prior authorization requirements.
Cost-benefit analysis extends beyond finances to include time commitment, side effect burden, and achieved symptom relief when comparing approaches.
Testosterone and Athletic Performance
Strength Gains and Recovery Enhancement
Adequate testosterone concentrations optimize muscle protein synthesis following resistance training stimuli. Recovery between sessions improves when hormonal milieu supports anabolic processes. Competitive athletes prioritize testosterone optimization within natural limits to maximize training adaptations.
Age-related testosterone decline partially explains reduced training capacity and prolonged recovery needs in masters athletes. Addressing this hormonal component preserves athletic performance longevity.
Endurance Considerations
While strength athletes clearly benefit from optimized testosterone, endurance athletes demonstrate more complex relationships. Excessive endurance training may suppress testosterone through chronic energy deficit and elevated cortisol. Periodized training preventing overtraining maintains hormonal balance.
Testosterone influences red blood cell production, affecting oxygen-carrying capacity relevant to endurance performance. Maintaining adequate levels supports aerobic adaptations without requiring supraphysiological concentrations.
The Anti-Doping Perspective
Competitive athletes subject to drug testing must distinguish between therapeutic optimization and performance-enhancing abuse. Many sports organizations permit TRT under therapeutic use exemptions when medically justified. Regulations vary across governing bodies.
Natural optimization strategies remain universally acceptable, emphasizing the importance of lifestyle approaches for competitive athletes concerned about anti-doping compliance.
Seasonal and Cyclical Hormone Patterns
Annual Testosterone Fluctuations
Research demonstrates subtle seasonal variation in testosterone levels, with peaks occurring during autumn months and nadirs in spring in northern hemisphere populations. The mechanisms potentially involve photoperiod effects on circadian biology. These variations typically remain within 10-20% of individual baseline.
Consistent measurement timing accounts for seasonal effects when monitoring long-term hormonal trends. Single measurements may reflect seasonal variation rather than true decline.
Daily Rhythmic Considerations
The circadian testosterone pattern peaks shortly after waking and gradually declines throughout the day. This diurnal rhythm influences optimal testing timing and may affect symptom severity patterns. Evening fatigue may partially reflect normal daily testosterone nadir.
Aligning demanding physical or cognitive tasks with morning hormonal peaks optimizes performance. Understanding natural rhythms informs realistic expectations about energy fluctuations.
Age-Related Rhythm Dampening
Testosterone circadian amplitude—the difference between peak and trough—decreases with aging. Older men demonstrate flatter daily patterns with reduced morning peaks. Strengthening circadian rhythms through consistent sleep-wake schedules and light exposure may restore some amplitude.
Diminished circadian differentiation contributes to symptom manifestations in aging men beyond average daily testosterone decline alone.
Frequently Asked Questions
What causes testosterone levels to drop after 40?
The hypothalamic-pituitary-testicular axis undergoes age-related changes, including decreased gonadotropin-releasing hormone secretion and reduced Leydig cell responsiveness to luteinizing hormone. Chronic inflammation within testicular tissue and increased oxidative stress further impair testosterone synthesis. Sex hormone-binding globulin increases with age, sequestering more testosterone in inactive bound forms.
These mechanisms combine to produce the characteristic 1-2% annual testosterone decline observed after forty.
How quickly can lifestyle changes increase testosterone naturally?
Sleep optimization and stress reduction can improve testosterone within 2-4 weeks, while resistance training effects accumulate over 8-12 weeks. Nutritional interventions correcting zinc or vitamin D deficiency demonstrate benefits within 4-8 weeks. Body composition changes requiring fat loss and muscle gain take 12-16 weeks to meaningfully impact testosterone levels.
Consistent implementation of multiple strategies produces additive effects exceeding individual interventions alone.
What testosterone level requires treatment?
Total testosterone below 300 ng/dL coupled with clinical symptoms generally warrants treatment consideration. However, free testosterone levels and symptom severity matter more than arbitrary thresholds. Some men remain asymptomatic at 250 ng/dL while others experience significant symptoms at 400 ng/dL.
Treatment decisions should incorporate symptom burden, comorbid conditions, and potential benefits versus risks rather than relying solely on numerical cutoffs.
Can exercise alone fix low testosterone after 40?
Resistance training increases testosterone both acutely and chronically, particularly when combined with adequate recovery and nutrition. Men with borderline deficiency and modifiable lifestyle factors may restore testosterone to satisfactory levels through exercise alone. Those with severe hypogonadism—levels below 200 ng/dL—typically require pharmaceutical intervention for adequate correction.
Exercise optimizes the body’s testosterone production capacity but cannot overcome complete testicular failure or severe hypothalamic-pituitary dysfunction.
Which foods boost testosterone most effectively?
Oysters provide exceptional zinc concentrations essential for testosterone synthesis. Fatty fish like salmon supply vitamin D and omega-3 fatty acids supporting hormonal production. Eggs contain cholesterol and vitamin D serving as testosterone precursors.
Other beneficial foods include spinach for magnesium, Brazil nuts for selenium, and avocados for monounsaturated fats. Focusing on micronutrient adequacy rather than individual superfoods produces optimal results.
Does sleep really affect testosterone production significantly?
The majority of daily testosterone production occurs during deep sleep stages, with peak levels occurring in early morning hours. Sleep restriction to five hours nightly for one week decreased testosterone by 10-15% in healthy men.
Chronic poor sleep quality or insufficient duration compounds age-related testosterone decline. Optimizing sleep represents one of the most impactful natural interventions for hormonal health.
What are the risks of testosterone replacement therapy?
TRT may cause polycythemia—excessive red blood cell production increasing thrombotic risk—requiring periodic hematocrit monitoring. It suppresses endogenous testosterone and spermatogenesis, inducing temporary infertility. Sleep apnea symptoms may worsen in susceptible individuals.
Contrary to popular belief, TRT does not cause prostate cancer but may accelerate pre-existing malignancies. Appropriate patient selection and monitoring minimizes risks while maximizing therapeutic benefits.
How long does it take to see results from TRT?
Libido improvements often manifest within 3-6 weeks of initiating therapy. Energy enhancement and mood stabilization demonstrate variable timelines, typically appearing within 4-8 weeks. Body composition changes—increased muscle mass and reduced fat—require 12-16 weeks.
Bone density improvements accumulate gradually over 6-12 months. Individual response rates vary based on baseline severity, dosing, and concurrent lifestyle factors.
Can stress alone cause low testosterone?
Chronic stress elevates cortisol, which directly suppresses the hypothalamic-pituitary-testicular axis. The body prioritizes survival physiology over reproductive function during prolonged stress states. This mechanism protects against competing metabolic demands but reduces testosterone as a consequence.
Stress management through exercise, adequate sleep, and mindfulness practices can restore testosterone suppressed by excessive cortisol. However, stress alone rarely accounts for profound hypogonadism requiring TRT.
Is testosterone therapy safe long-term?
Decades of clinical use demonstrate acceptable safety profiles when prescribed appropriately with regular monitoring. Cardiovascular risks previously attributed to TRT have been challenged by more rigorous recent research. Long-term users require surveillance for polycythemia, prostate health, and lipid changes.
The safety profile depends on patient selection—excluding men with contraindications—and consistent medical oversight. Many men continue TRT indefinitely without significant complications when properly managed.
Take Control of Your Hormonal Destiny
Understanding testosterone after 40 empowers men to implement evidence-based strategies that restore vitality, strength, and mental clarity. The gradual hormonal decline beginning around forty need not dictate your quality of life. Strategic resistance training, micronutrient optimization, and sleep architecture improvements form the foundation of natural testosterone enhancement.
These lifestyle interventions offer additional health benefits extending far beyond androgen levels alone. Cardiovascular fitness improves, metabolic dysfunction reverses, and mental acuity sharpens through the same practices supporting hormonal balance. For men requiring pharmaceutical intervention, combining TRT with lifestyle optimization maximizes therapeutic outcomes while minimizing risks.
Your hormonal health deserves the same attention you dedicate to other aspects of wellness. Consult qualified healthcare providers who understand the nuances of testosterone after 40 management. Annual screening enables early detection of concerning declines, allowing intervention before severe deficiency develops. The investment in hormonal optimization pays dividends across physical, mental, and social dimensions of masculine well-being throughout your remaining decades. Click here for more Testosterone Balance guide.