Your occupation might be silently sabotaging your cardiovascular system. Recent epidemiological investigations demonstrate that chronic work stress heart complications affect millions of professionals globally, with prospective observational studies revealing a 40-50% elevation in coronary disease incidence among persistently stressed employees.
The physiological toll extends far beyond temporary fatigue, manifesting as genuine pathological transformations within your cardiac architecture. Understanding these mechanisms empowers you to recognize warning signals before irreversible damage crystallizes.
Elevated Blood Pressure Through Sympathetic Activation
Sustained Hypertensive States
The neuroendocrine cascade triggered by occupational strain precipitates a persistent elevation of arterial pressure.
Job strain, characterized by high demands coupled with minimal decisional latitude, initiates chronic sympathoadrenal activation that fundamentally resets your circadian blood pressure profile.
This phenomenon transcends temporary workplace spikes, maintaining elevated readings during sleep and leisure periods.
Research demonstrates that workers experiencing chronic work stress heart complications exhibit significantly higher systolic and diastolic measurements across all daily periods.
The pathophysiology involves hypersecretion of cortisol, which disrupts the hypothalamic-pituitary-adrenal axis’s harmful feedback mechanisms. This hormonal dysregulation promotes arterial wall hardening through atherosclerotic processes.
Impaired Cardiovascular Recovery
Delayed physiological recuperation represents another critical mechanism connecting occupational strain to hypertension.
Studies using ambulatory monitoring reveal that stressed employees exhibit prolonged heart rate elevation extending beyond workplace departure. The inability to achieve adequate parasympathetic rebound intensifies cumulative cardiovascular burden.

Inflammatory Cascade Amplification
Cytokine Upregulation Mechanisms
Occupational psychosocial stressors activate inflammatory pathways that directly assault cardiovascular integrity. The chronic work stress heart connection operates through cortisol-mediated immune dysregulation, wherein excessive hormone secretion paradoxically diminishes anti-inflammatory capacity. This creates susceptibility to atherosclerotic plaque formation.
High-sensitivity C-reactive protein concentrations are significantly elevated among employees experiencing job strain, and these levels correlate with coronary calcification scores. The biological cascade involves macrophage activation, platelet aggregation facilitation, and inflammatory cytokine upregulation. These molecular events constitute fundamental mechanisms underlying stress-induced cardiovascular pathogenesis.
Endothelial Dysfunction Progression
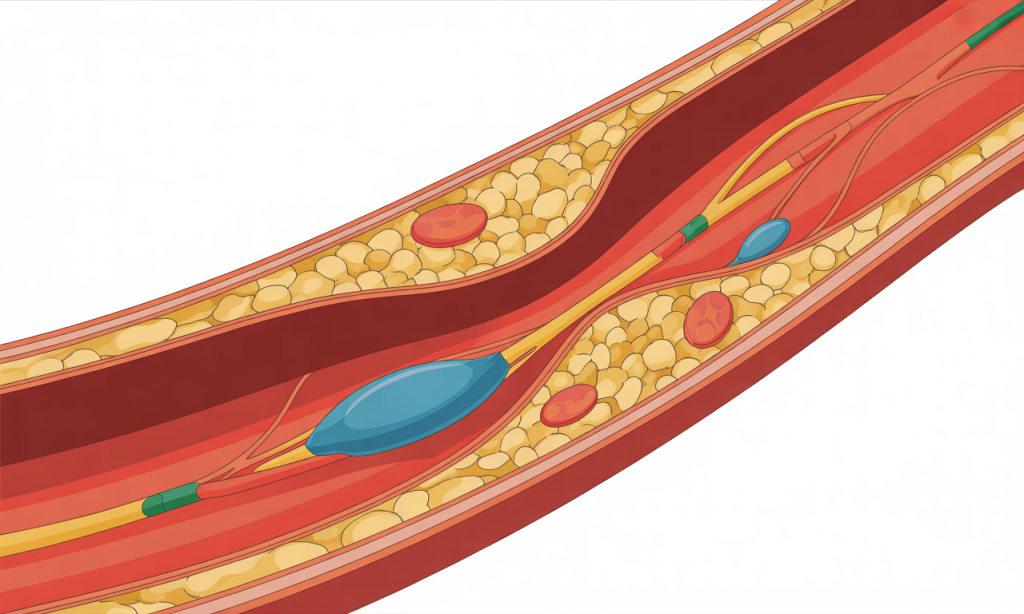
The vascular endothelium—your blood vessels’ protective inner lining—sustains significant damage from prolonged occupational stress. Research examining endothelial dysfunction markers reveals that chronic work stress heart effects include impaired nitric oxide bioavailability and increased endothelin-1 production. This imbalance promotes vasoconstriction and reduces arterial compliance.
Reactive oxygen species generation accelerates under persistent stress conditions, compromising endothelial cell function. The resulting oxidative damage initiates atherogenic transformations that predispose individuals to acute coronary syndromes. Biomarker analyses demonstrate significant associations between job strain and augmented vascular inflammation indices.
Coronary Artery Disease Development
Atherosclerotic Plaque Accumulation
The architectural integrity of your coronary circulation deteriorates progressively under sustained occupational pressure. Meta-analytical evidence indicates approximately 50% excess risk for coronary heart disease among workers experiencing chronic job strain. This statistical elevation reflects genuine pathological alterations within arterial structures.
Job strain accelerates atherosclerosis through multiple converging pathways, including disruption of lipid metabolism and chronic inflammatory activation. Studies utilizing coronary calcification scoring methodologies demonstrate statistically significant associations between psychosocial work factors and calcium deposition severity. These anatomical changes represent tangible manifestations of stress-induced vascular injury.
Myocardial Ischemia Risk
Insufficient oxygen delivery to cardiac muscle tissue represents a lethal consequence of chronic work stress heart pathology. The combination of increased myocardial oxygen demand—driven by elevated heart rate and blood pressure—with reduced supply capacity creates dangerous ischemic conditions. Research demonstrates that effort-reward imbalance doubles normal coronary artery disease risk.
The rate-pressure product, calculated from systolic pressure and heart rate measurements, provides quantification of myocardial oxygen consumption. Chronically stressed workers exhibit significantly elevated rate-pressure products, indicating sustained cardiac workload amplification. This metabolic strain predisposes individuals to angina pectoris and myocardial infarction events.
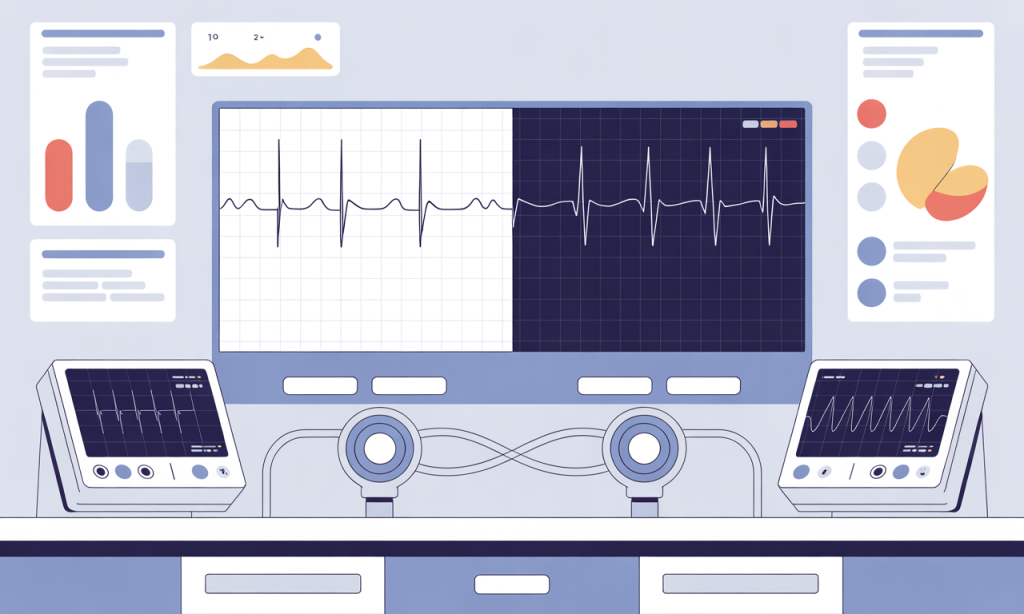
Arrhythmia Susceptibility Enhancement
Atrial Fibrillation Incidence
Irregular cardiac electrical conduction patterns emerge with disturbing frequency among chronically stressed professionals. Groundbreaking research published in the Journal of the American Heart Association reveals that workers experiencing both high job strain and effort-reward imbalance demonstrate 97% increased atrial fibrillation risk compared to minimally stressed peers. This represents nearly a doubling of the probability of developing this dangerous arrhythmia.
The pathophysiological underpinnings involve autonomic nervous system dysregulation, in which excessive sympathetic tone disrupts the maintenance of normal sinus rhythm. Catecholamine surges—epinephrine and norepinephrine—create electrophysiological instability within atrial tissue. Job strain alone associates with 83% higher AFib risk, while effort-reward imbalance confers 44% elevation.
Sympathovagal Imbalance
Heart rate variability analysis reveals profound autonomic dysfunction among individuals experiencing chronic work stress heart complications. Specifically, the ratio of low- to high-frequency power spectral components is significantly elevated, indicating sympathetic predominance with vagal withdrawal. This imbalance compromises cardiac electrical stability.
Research utilizing continuous ambulatory monitoring documents that effort-reward imbalance correlates with diminished 24-hour vagal tone across all measurement periods. Reduced parasympathetic modulation eliminates protective influences that normally buffer against arrhythmogenic triggers. The resulting autonomic dysfunction substantially amplifies ventricular dysrhythmia susceptibility.
Accelerated Biological Aging
Epigenetic Age Advancement
Your chronological age diverges increasingly from your physiological age under sustained occupational pressure. Investigation of epigenetic markers utilizing the PhenoAge clock reveals that chronic work stress heart effects extend to cellular aging acceleration. Workers experiencing high job strain demonstrate significantly advanced biological ages compared to calendar years.
The association proves dose-dependent, with progressively worsening chronic health condition trajectories correlating to epigenetic age advancement. After controlling for demographic variables, elevated PhenoAge associates with four-fold increased risk of classification into the worst chronic health trajectory category. Importantly, job stress partially mediates this relationship, explaining observable associations between accelerated aging and disease accumulation.
Telomere Length Reduction
Chromosomal protective structures called telomeres undergo accelerated shortening under persistent psychosocial strain. These repetitive DNA sequences safeguard genetic integrity during cellular replication, with their length serving as a a biomarker of biological aging. Research examining night shift workers—who experience compounded occupational stress—reveals significant telomere attrition alongside elevated chronic disease prevalence.
The mechanistic pathway involves oxidative stress amplification and inflammatory activation, both consequences of chronic work stress heart pathology. Shortened telomeres compromise cellular regenerative capacity within cardiovascular tissues, accelerating degenerative processes. This molecular aging mechanism contributes substantially to premature cardiovascular disease manifestation among stressed workers.
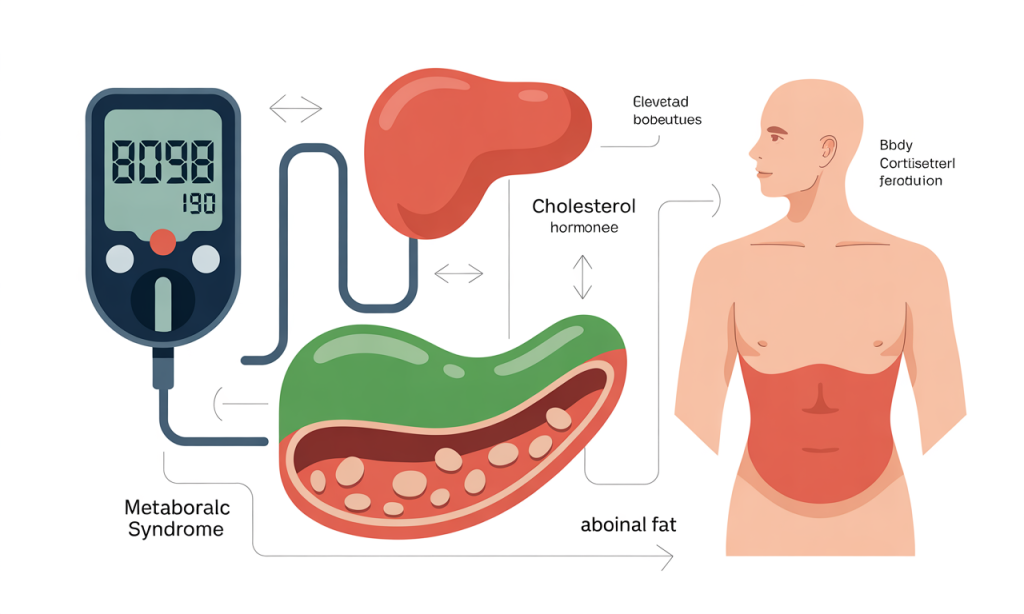
Metabolic Syndrome Components
Glucose Dysregulation
Chronic cortisol hypersecretion fundamentally disrupts carbohydrate metabolism and insulin sensitivity. The chronic work stress heart connection extends beyond direct cardiac effects to encompass comprehensive metabolic derangements. Elevated stress hormone concentrations increase blood glucose levels through hepatic gluconeogenesis stimulation and peripheral insulin resistance induction.
Prospective studies document significant associations between job strain and incident type 2 diabetes development. The metabolic dysfunction creates additional cardiovascular risk through multiple mechanisms, including glycosylation of vascular proteins and promotion of dyslipidemia. This represents a synergistic pathological cascade wherein stress-induced metabolic abnormalities compound direct cardiac damage.
Lipid Profile Deterioration
Triglyceride elevation and high-density lipoprotein reduction characterize the dyslipidemic pattern observed among chronically stressed professionals. Research demonstrates that sustained cortisol excess promotes unfavorable alterations across multiple lipid parameters. These changes accelerate atherogenic processes within the coronary circulation.
The effort-reward imbalance model particularly correlates with metabolic syndrome prevalence, encompassing abdominal adiposity, hypertension, glucose intolerance, and dyslipidemia. This constellation of risk factors dramatically amplifies cardiovascular disease probability. Addressing occupational psychosocial stressors therefore provides leverage for comprehensive metabolic risk reduction.
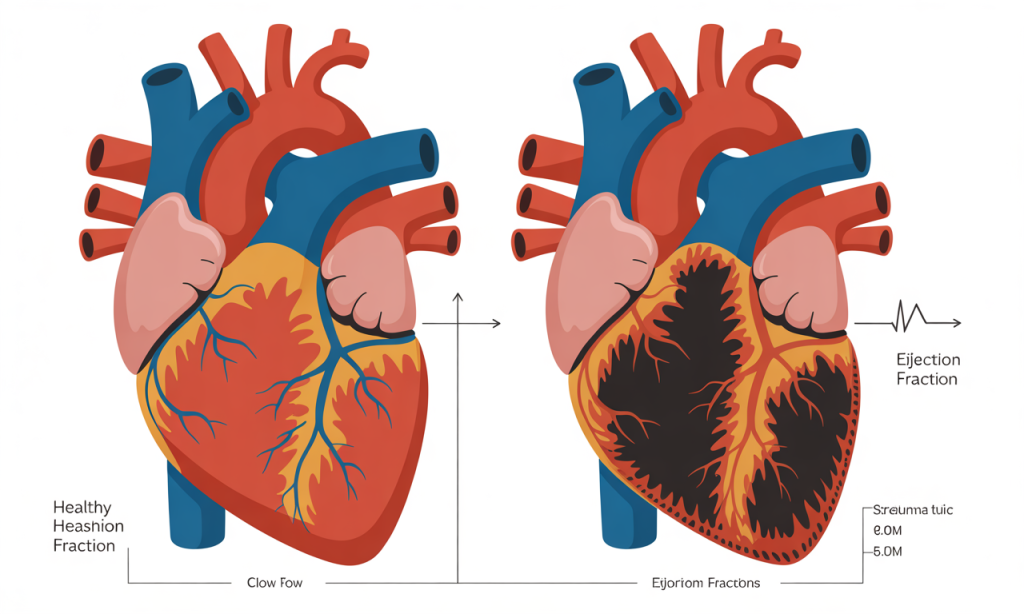
Myocardial Remodeling
Sustained hemodynamic burden imposed by stress-induced hypertension precipitates structural cardiac alterations. Left ventricular hypertrophy develops as compensatory response to chronically elevated afterload, progressively compromising cardiac efficiency. Research examining organizational justice and job strain models confirms associations with cardiovascular mortality, partially mediated through heart failure pathways.
The chronic work stress heart relationship manifests through continuous activation of neurohormonal systems that promote adverse myocardial remodeling. Angiotensin II levels remain persistently elevated, stimulating fibroblast proliferation and collagen deposition within cardiac muscle. This fibrotic transformation reduces ventricular compliance and impairs diastolic filling dynamics.
Reduced Ejection Fraction
Systolic dysfunction emerges as the cumulative damage from multiple stress-mediated pathways converges. The combination of ischemic injury, inflammatory damage, autonomic dysregulation, and metabolic derangements progressively undermines contractile performance. Population-based studies document elevated heart disease incidence rates among workers experiencing chronic psychosocial occupational stressors.
The transition from compensated to decompensated states often occurs precipitously, triggered by acute stressors superimposed upon chronically damaged myocardium. Biomarker evidence demonstrates that job strain correlates with elevated natriuretic peptide concentrations, indicating subclinical cardiac dysfunction. Early recognition and intervention prove critical for preventing irreversible heart failure progression.
Frequently Asked Questions
How does chronic work stress heart damage develop over time?
The pathological progression occurs through sustained activation of stress hormone systems, notably cortisol and catecholamines, which trigger inflammatory cascades and sympathetic nervous system overactivity. These biological responses initially serve protective functions but become destructive when perpetually engaged. Over months and years, the cumulative burden manifests as hypertension, atherosclerosis, arrhythmias, and eventually structural cardiac damage including myocardial remodeling and heart failure.
What blood pressure changes indicate chronic work stress heart effects?
Ambulatory monitoring typically reveals elevated readings across all daily periods—not just during work hours—with systolic pressures increasing 14-16 mmHg above baseline among highly stressed workers. The persistent elevation during sleep periods proves particularly concerning, as healthy individuals commonly experience nocturnal blood pressure dipping. Absent or blunted nocturnal reduction serves as powerful predictor of cardiovascular events and indicates chronic stress-mediated autonomic dysfunction requiring intervention.
Can reducing workplace stress reverse chronic work stress heart damage?
Organizational interventions designed to minimize psychosocial stressors demonstrate measurable cardiovascular benefits, including blood pressure reduction and improved autonomic function. Implementation strategies encompass flexible scheduling, workload management through project pacing adjustments, and enhanced employee decision-making participation. While early-stage functional abnormalities often prove reversible with stress reduction, advanced structural changes like significant ventricular hypertrophy or established atherosclerotic disease may persist despite intervention, underscoring prevention importance.
What cortisol levels indicate dangerous chronic work stress heart risk?
Research demonstrates that chronically elevated cortisol concentrations—whether measured by 24-hour urinary excretion or multiple salivary samples—associate with a 60% increase in cardiovascular risk. The pattern matters beyond absolute values, with flattened diurnal rhythms indicating hypothalamic-pituitary-adrenal axis dysregulation.
Workers experiencing effort-reward imbalance often exhibit this pattern alongside gradually declining catecholamine levels despite ongoing stress exposure, signaling psychophysiological exhaustion and heightened cardiac vulnerability.
How does job strain differ from general life stress regarding cardiac effects?
Job strain specifically combines high psychological demands with low decisional latitude, creating unique physiological signature distinct from other stressors. This particular configuration produces more consistent cardiovascular consequences than general life stress, potentially because occupational exposures recur daily throughout working years.
Meta-analyses reveal approximately 50% excess coronary heart disease risk specifically attributable to job strain, independent of traditional risk factors. The sustained, predictable nature of workplace stress prevents adequate recovery periods, which are essential for physiological restoration.
What inflammation markers reveal chronic work stress heart damage?
High-sensitivity C-reactive protein elevation represents the most consistently documented inflammatory biomarker, with job strain correlating to significantly elevated concentrations. Additional markers include increased interleukin-6, tumor necrosis factor-alpha, and other pro-inflammatory cytokines released through stress-activated immune pathways.
Fndothelial dysfunction markers such as impaired flow-mediated dilation and elevated endothelin-1 provide functional assessment of vascular injury. Comprehensive panels incorporating multiple inflammatory and endothelial markers offer superior risk stratification compared to single measurements.
Does chronic work stress affect heart disease in women differently than in men?
Research reveals concerning gender disparities, with some studies demonstrating stronger associations in male populations while others document equivalent or greater effects among women. Men experiencing effort-reward imbalance demonstrate doubled heart disease risk comparable to obesity’s impact.
However, women remain understudied in cardiovascular stress research, with only one-third of investigations including substantial female representation. Hormonal influences, occupational role differences, and coping strategy variations likely modulate stress-cardiac relationships differently across genders, warranting targeted investigation.
What heart rhythm abnormalities result from workplace stress?
Atrial fibrillation represents the most extensively documented arrhythmia, with combined job strain and effort-reward imbalance conferring 97% increased risk. The mechanistic pathway involves catecholamine-induced electrophysiological instability coupled with autonomic imbalance favoring sympathetic predominance.
Additional rhythm disturbances include premature ventricular contractions, supraventricular tachycardias, and in severe cases, life-threatening ventricular arrhythmias. Heart rate variability analysis reveals characteristic patterns of reduced vagal tone that predispose to these electrical conduction abnormalities.
How quickly do cardiovascular changes occur after workplace stress exposure begins?
Acute physiological responses manifest within hours, including blood pressure elevation and heart rate acceleration persisting beyond work periods. However, pathological transformations requiring clinical intervention typically develop across months to years of sustained exposure.
Prospective cohort investigations following workers over 18-year periods document cumulative incidence patterns, with risk escalating progressively alongside exposure duration. Early biomarker abnormalities—including inflammatory marker elevation and endothelial dysfunction—often precede clinical disease manifestation by years, enabling preventive intervention opportunities.
What prevention strategies effectively protect against chronic work stress heart complications?
Evidence-based approaches encompass both organizational and individual interventions, with workplace-level modifications demonstrating superior efficacy.
Organizational strategies include implementing flexible schedules, reducing excessive workloads by setting realistic deadlines, enhancing employee autonomy in decision-making, and ensuring an equitable effort-reward balance through appropriate compensation and recognition systems.
Individual tactics incorporate regular aerobic exercise to metabolize stress hormones, mindfulness-based stress reduction techniques, adequate sleep prioritization, and social support cultivation. Comprehensive programs addressing multiple levels simultaneously achieve optimal cardiovascular protection.
Protecting Your Cardiac Health From Occupational Hazards
The mounting evidence linking chronic work stress to heart pathology and substantial morbidity and mortality demands immediate attention from both employees and employers. Your cardiovascular system lacks unlimited resilience against perpetual psychosocial strain.
Recognition of warning signs including persistent hypertension, unexplained fatigue, palpitations, or chest discomfort warrants thorough medical evaluation incorporating stress assessment.
Implementing protective strategies need not await perfect workplace conditions. Begin incorporating stress-buffering behaviors today—establish firm boundaries between professional and personal time, prioritize regular physical activity, cultivate supportive relationships, and advocate for organizational changes that promote sustainable work practices. Your heart’s future depends upon actions initiated now.
Explore our comprehensive resources on workplace wellness strategies, cardiovascular risk assessment tools, and stress management techniques.
Discover evidence-based approaches for negotiating healthier work arrangements and implementing daily practices that shield your heart from occupational damage. Your cardiovascular longevity merits investment in both personal resilience and systemic workplace improvements.

