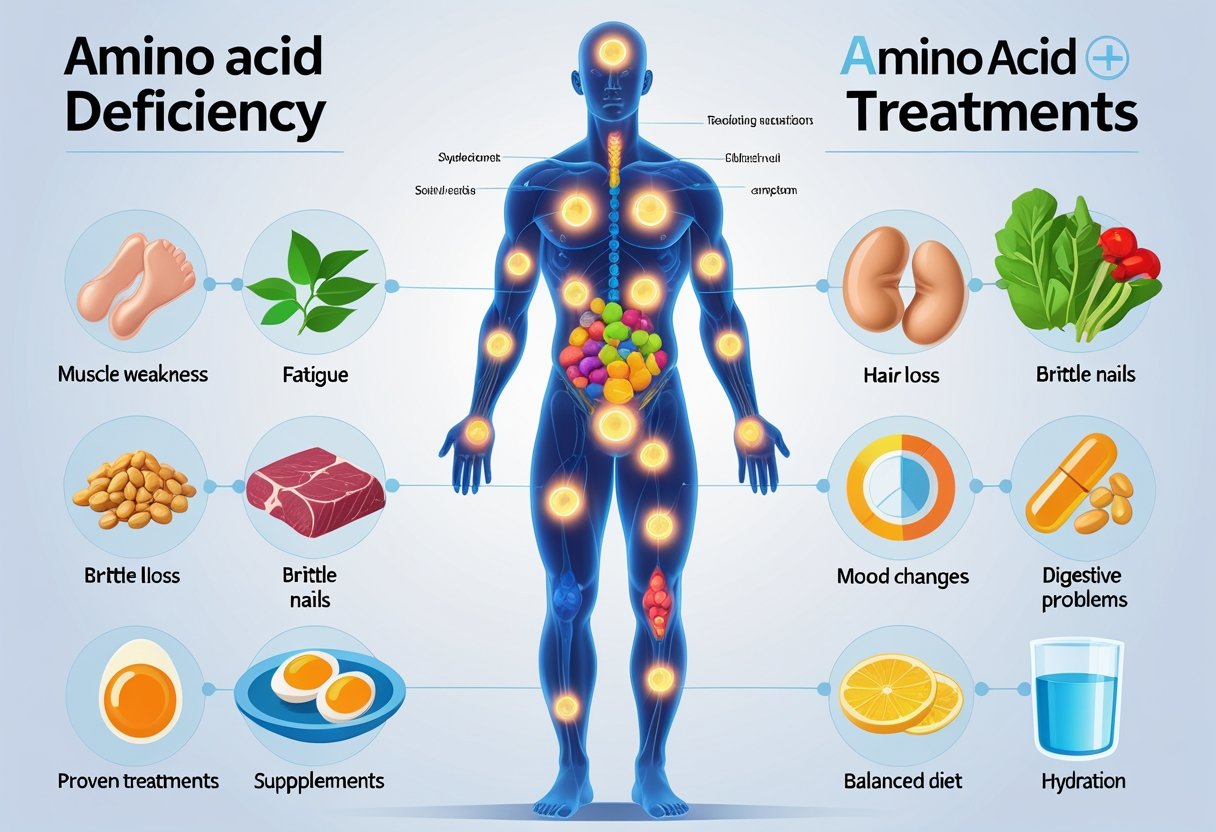
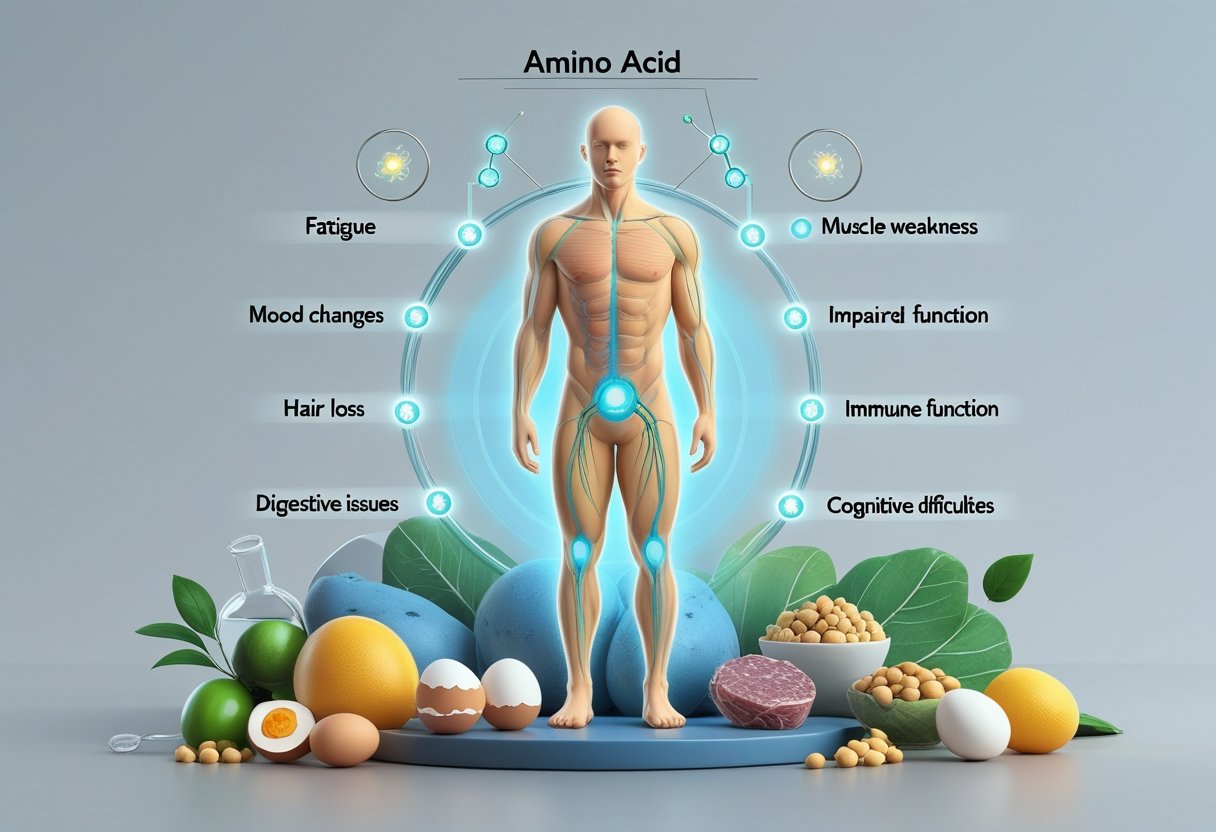
Feeling tired, noticing changes in your skin, or experiencing mood swings might be more than just daily stress—these could be signs of an amino acid deficiency. Amino acids are the building blocks of proteins that perform essential functions in the body, from supporting muscle growth to regulating mood and immune function.
When the body lacks sufficient amino acids, it can manifest in several warning signs including swelling in the abdomen and extremities, muscle loss, and even premature aging symptoms. These symptoms often develop gradually, making them easy to overlook or attribute to other conditions.
Understanding these warning signs can help identify deficiencies early and implement effective treatments through dietary changes, supplements, or medical interventions. With proper diagnosis and treatment, most people can restore their amino acid balance and improve their overall health and well-being.
Key Takeaways
- Amino acid deficiencies can cause visible symptoms like swelling, skin problems, and muscle loss that affect daily functioning and long-term health.
- Both genetic factors and dietary habits play significant roles in developing amino acid imbalances, with certain populations at higher risk.
- Early detection through recognition of warning signs and appropriate testing allows for targeted nutritional and medical interventions that can effectively reverse deficiency symptoms.
Understanding Amino Acids and Their Role in Health
Amino acids form the building blocks of protein in the human body and play crucial roles in numerous physiological processes. These compounds support everything from muscle growth to immune function and brain health.
What Are Amino Acids?
Amino acids are organic compounds that combine to form proteins, which are vital for nearly every biological process in the body. Each amino acid contains an amino group, a carboxyl group, and a side chain that is unique to each type.
These powerful compounds serve as the building blocks for enzymes, hormones, and neurotransmitters. They're essential for:
- Protein synthesis and muscle repair
- Immune system function
- Metabolism regulation
- Neurotransmitter production
- Tissue growth and repair
The human body uses amino acids not just for building proteins but also for creating energy when needed. Without sufficient amino acids, many bodily functions would decline or fail completely.
Types of Amino Acids: Essential vs. Non-essential
Amino acids fall into two main categories based on whether the body can produce them or must obtain them through diet.
Essential amino acids cannot be synthesized by the human body and must come from food sources. The nine essential amino acids include:
- Histidine
- Isoleucine
- Leucine
- Lysine
- Methionine
- Phenylalanine
- Threonine
- Tryptophan
- Valine
Non-essential amino acids can be produced by the body, making them unnecessary to include in diet. These include alanine, asparagine, aspartic acid, and glutamic acid among others.
Conditionally essential amino acids become necessary during illness or stress when the body cannot produce sufficient amounts. Examples include arginine and glutamine.
Amino Acid Metabolism Explained
Amino acid metabolism involves complex processes through which the body breaks down, transforms, and utilizes these compounds.
When we consume protein, digestive enzymes break it down into individual amino acids. These amino acids enter the bloodstream and travel to cells where they're used to:
- Build new proteins specific to cellular needs
- Create energy when carbohydrates aren't available
- Synthesize other compounds like neurotransmitters
The liver plays a central role in amino acid metabolism, managing the amino acid pool through processes like transamination and deamination. Excess amino acids cannot be stored, so they're converted to glucose or fat.
BCAAs (branched-chain amino acids) – leucine, isoleucine, and valine – have special metabolic pathways. They're primarily metabolized in muscle tissue rather than the liver, making them particularly important for muscle function and recovery.
Key Causes and Risk Factors of Amino Acid Deficiency
Amino acid deficiencies arise from several distinct sources ranging from genetic factors to dietary choices and underlying health conditions. These deficiencies can significantly impact overall health as amino acids are essential building blocks for proteins and important neurotransmitters in the body.
Inherited Metabolic Disorders
Inherited metabolic disorders represent a major cause of amino acid deficiencies due to genetic mutations that affect protein metabolism. Phenylketonuria (PKU) is one of the most common disorders, where the body cannot properly break down the amino acid phenylalanine, leading to harmful buildup.
Other significant genetic disorders include:
- Maple Syrup Urine Disease: Prevents proper breakdown of branched-chain amino acids
- Homocystinuria: Disrupts methionine metabolism
- Tyrosinemia: Affects tyrosine processing
These conditions are typically identified during newborn screening programs. Children with these metabolic disorders often require special diets and medical supervision throughout life. Early detection remains crucial as untreated cases can lead to severe developmental delays and neurological damage.
Dietary Causes and Malnutrition
Poor dietary choices represent a common pathway to amino acid deficiencies, particularly for essential amino acids that cannot be produced by the body. Inadequate protein intake is especially problematic for vegetarians and vegans who don't carefully plan their meals.
Protein requirements increase during:
- Pregnancy and breastfeeding
- Periods of rapid growth
- Recovery from illness or injury
- Intense athletic training
Malabsorption conditions like Crohn's disease or celiac disease can prevent proper amino acid absorption even with adequate dietary intake. Economic factors also play a role, as food insecurity leads to limited protein variety and quantity.
Signs of dietary-related deficiency often develop gradually, with changes in brain function being among the concerning symptoms as neurotransmitter production depends on specific amino acids.
Medical Conditions and Renal Failure
Certain medical conditions directly impact amino acid metabolism and utilization. Renal failure is particularly significant as kidneys regulate amino acid levels in the bloodstream. When kidneys fail, amino acid imbalances occur in both directions – some increase to toxic levels while others become depleted.
Burns and severe infections cause hypermetabolism, dramatically increasing amino acid requirements. The body often breaks down muscle tissue to meet these needs if dietary sources are insufficient.
Conditions that affect amino acid processing include:
- Liver disease: Impairs protein metabolism
- Cystic fibrosis (CF): Affects nutrient absorption
- Sickle cell anemia: Increases protein breakdown
- Congenital adrenal hyperplasia: Alters amino acid utilization
Medications can also interfere with amino acid metabolism, particularly certain antibiotics, chemotherapy drugs, and anti-seizure medications. Patients with these conditions require specialized nutritional approaches and regular monitoring of amino acid profiles.
7 Warning Signs of Amino Acid Deficiency
Amino acid deficiencies can manifest through various physical and cognitive symptoms. These deficiencies impact critical bodily functions since amino acids are essential building blocks for proteins that support brain development, energy production, and overall health.
Developmental Delay and Intellectual Disability
Children with amino acid deficiencies often show signs of stunted growth and developmental delays. This is particularly evident in conditions like Phenylketonuria (PKU), where the body cannot properly process the amino acid phenylalanine.
In severe cases, untreated amino acid deficiencies can lead to intellectual disability. Brain development relies heavily on proper amino acid balance, especially during the crucial early years of life.
Physical manifestations may include delayed walking or talking milestones. Children might not reach growth benchmarks at expected ages, indicating potential nutritional insufficiencies.
Early intervention is critical. Most developed countries now screen newborns for PKU and other amino acid disorders to prevent these developmental complications through dietary management and supplementation.
Fatigue and Cognitive Decline
Persistent fatigue that doesn't improve with rest may indicate amino acid deficiency. Amino acids help produce energy within cells, and shortages can lead to constant tiredness.
Cognitive functions often decline with amino acid imbalances. People may experience:
- Memory problems
- Difficulty concentrating
- Mental fog
- Reduced problem-solving abilities
The brain relies on amino acids to produce neurotransmitters like serotonin and dopamine. Without sufficient amino acids, cognitive processes slow down and become less efficient.
Recovery from mental exertion takes longer when amino acid levels are inadequate. Many people report increased mental clarity after addressing these nutritional deficiencies through diet or supplementation.
Seizures and Neurological Symptoms
Severe amino acid deficiencies can trigger neurological symptoms, including seizures. This is especially common in disorders where amino acid metabolism is impaired.
Brain function depends on balanced neurotransmitters, which require specific amino acids for production. When these building blocks are missing, electrical activity in the brain can become irregular.
Other neurological symptoms may include:
- Tremors
- Muscle weakness
- Poor coordination
- Numbness or tingling sensations
Amino acid deficiencies can also impact the peripheral nervous system. Some people experience strange sensations in their extremities or difficulty with fine motor control.
In children, these neurological manifestations may be mistaken for other conditions. Proper diagnosis requires specialized testing to identify specific amino acid imbalances.
Behavioral Problems and Mood Changes
Amino acid deficiencies can significantly impact mood regulation and behavior. Children with these deficiencies may display irritability, aggression, or withdrawal.
Depression and anxiety often accompany amino acid imbalances. This connection exists because many neurotransmitters that regulate mood require specific amino acids as precursors.
Common behavioral changes include:
- Sudden mood swings
- Increased irritability
- Poor stress management
- Sleep disturbances
In conditions like PKU, behavioral symptoms can become more pronounced when dietary restrictions aren't followed. The accumulated phenylalanine affects brain chemistry, leading to noticeable personality changes.
Addressing the underlying amino acid deficiency often improves these behavioral symptoms. Proper nutrition therapy can help stabilize mood and reduce problematic behaviors.
Additional Symptoms Associated With Amino Acid Deficiency
Amino acid deficiencies can manifest in various bodily systems beyond the common symptoms of fatigue and muscle weakness. These deficiencies can affect sensory functions, cardiovascular health, and physical development, particularly in growing children.
Hearing Loss and Speech Problems
Certain amino acid deficiencies are linked to developmental disabilities that affect hearing and speech. Phenylalanine, tyrosine, and tryptophan deficiencies may impact the production of neurotransmitters necessary for auditory processing.
Children with untreated phenylketonuria (PKU), an amino acid metabolism disorder, often develop speech delays and hearing problems. These issues occur because the brain lacks essential proteins needed for proper auditory pathway development.
Early symptoms include:
- Delayed speech development
- Difficulty processing verbal instructions
- Progressive hearing loss
- Trouble with sound localization
Early detection through newborn screening is critical, as many hearing and speech problems can be prevented with proper dietary management and amino acid supplementation.
Heart Defects and Stroke
Amino acid imbalances can significantly impact cardiovascular health. Homocysteine, an amino acid byproduct, becomes elevated when there are deficiencies in methionine metabolism.
High homocysteine levels damage blood vessel walls and promote blood clotting, increasing stroke risk. Studies show that deficiencies in the amino acids taurine and carnitine are associated with heart muscle weakness.
Congenital heart defects may also result from maternal amino acid deficiencies during pregnancy. These structural abnormalities can include:
- Septal defects (holes between heart chambers)
- Valve malformations
- Narrowed arteries
Regular cardiovascular screening is recommended for individuals with known amino acid metabolism disorders to monitor heart function and prevent complications.
Growth Issues in Newborns and Children
Amino acid metabolism disorders frequently present with growth problems in children. When the body cannot properly process essential amino acids, protein synthesis for growth is compromised.
Infants with these disorders often show:
- Failure to thrive
- Below-average height and weight
- Delayed developmental milestones
- Abnormal bone formation
Maple syrup urine disease and other amino acid disorders require early intervention to prevent permanent growth impairment. Newborn screening programs now test for many of these conditions, allowing for prompt treatment.
Treatment typically involves special diets limiting specific amino acids, medical formulas, and careful monitoring of growth parameters. With proper management, many children can achieve normal or near-normal growth patterns despite their underlying metabolic condition.
Genetic and Newborn Screening for Amino Acid Disorders

Early detection of amino acid disorders through newborn screening is crucial for preventing serious health complications. These screening programs have become standard practice in healthcare systems worldwide, helping identify conditions before symptoms appear.
Understanding Newborn Screening
Newborn screening for amino acid disorders involves taking a small blood sample from a baby's heel, typically 24-48 hours after birth. This sample is analyzed for abnormal levels of amino acids and related compounds. Most babies who have follow-up testing for amino acid disorders are healthy, but the screening can identify those at risk.
In the United States, all states conduct newborn screening for various conditions, including amino acid disorders, fatty acid oxidation disorders, and other metabolic conditions. The specific disorders screened vary by state but typically include:
- Phenylketonuria (PKU)
- Maple Syrup Urine Disease (MSUD)
- Homocystinuria
- Tyrosinemia
Early identification allows for prompt intervention, often preventing intellectual disability and other serious complications.
Diagnostic Testing and Interpretation
When newborn screening results suggest a possible amino acid disorder, follow-up diagnostic testing is necessary. These tests are more comprehensive and may include:
- Blood plasma amino acid analysis
- Urine organic acid testing
- Genetic testing for specific mutations
The buildup of amino acids or their metabolites in the blood can cause severe medical complications. Interpretation of results requires specialized knowledge, as many factors can affect amino acid levels, including:
- Nutritional status
- Liver function
- Medication use
- Collection timing
False positives do occur, which is why confirmatory testing is essential. Parents should understand that an abnormal screening result doesn't necessarily mean their child has a disorder.
The Role of IRT and Biochemical Analysis
Immunoreactive trypsinogen (IRT) testing, combined with biochemical analysis, forms the cornerstone of comprehensive metabolic screening. While IRT is primarily associated with cystic fibrosis screening, similar enzymatic and biochemical approaches are used for amino acid disorders.
Advanced laboratory techniques can detect subtle metabolic abnormalities that indicate an amino acid disorder. These include:
- Tandem mass spectrometry (MS/MS)
- High-performance liquid chromatography (HPLC)
- Gas chromatography-mass spectrometry (GC-MS)
Warning signs that may prompt testing outside of newborn screening include low energy, vomiting, fever, and behavioral changes. These symptoms can appear when a child faces metabolic stress such as illness or fasting.
Biochemical analysis results guide treatment decisions, including specialized diets, supplements, and medications designed to manage specific amino acid imbalances.
Common Inherited Amino Acid Disorders
Several genetic conditions affect how our bodies process amino acids, leading to serious health problems when harmful substances build up. These disorders are often detected through newborn screening and require lifelong management.
Phenylketonuria (PKU) and Its Symptoms
Phenylketonuria, commonly known as PKU, is an inherited metabolic disorder where the body cannot properly break down the amino acid phenylalanine. This causes phenylalanine to accumulate to harmful levels in the blood and brain.
The most common symptoms of PKU include:
- Delayed development or intellectual disability
- Behavioral problems and psychiatric disorders
- Seizures
- Skin rashes (eczema)
- Musty or “mousy” body odor
- Fair skin and blue eyes (due to pigment issues)
- Smaller head size (microcephaly)
If left untreated, PKU can cause severe brain damage. The good news is that with early detection through newborn screening and proper treatment—primarily a special diet low in phenylalanine—most people with PKU can lead normal, healthy lives.
Maple Syrup Urine Disease
Maple syrup urine disease is a rare condition where the body cannot process certain amino acids (leucine, isoleucine, and valine). The name comes from the sweet, maple syrup smell of the urine in affected individuals.
Symptoms typically appear within the first week of life and include:
- Sweet-smelling urine
- Poor feeding and vomiting
- Lethargy and poor muscle tone
- Seizures
- Developmental delays
- Coma if untreated
This condition requires immediate treatment to prevent brain damage and death. Management includes a specialized diet restricting the problematic amino acids and careful monitoring during illness or stress, as these can trigger metabolic crises.
Methylmalonic Acidemia and Propionic Acidemia
These related amino acid metabolism disorders prevent the body from properly processing certain amino acids and fats. Both conditions involve defects in enzymes needed for protein metabolism.
Key characteristics include:
- Vomiting
- Dehydration
- Extreme tiredness
- Weak muscle tone
- Growth failure
- Intellectual disabilities
These disorders often present in the newborn period with metabolic acidosis—a dangerous change in body chemistry. Treatment involves a protein-restricted diet, special medical formulas, and supplements. Some patients benefit from vitamin B12 injections (particularly for methylmalonic acidemia).
During illness, patients may need hospitalization for IV fluids and close monitoring to prevent metabolic crises. In severe cases, liver transplantation may be considered for methylmalonic acidemia.
Nutritional And Therapeutic Interventions
Treating amino acid deficiencies requires a targeted approach combining dietary modifications and specific supplementation strategies. Proper management often involves medical supervision to ensure nutritional needs are met while addressing the underlying metabolic issues.
Special Diets and Low-Protein Diets
A low-protein diet is often prescribed for certain amino acid disorders, particularly those involving ammonia buildup. These diets help reduce the production of toxic metabolites while ensuring adequate nutrition.
For urea cycle disorders (UCDs), protein restriction is crucial to manage ammonia levels. Doctors typically calculate the exact amount of protein a patient can safely consume.
Medical food products designed for specific amino acid disorders provide essential nutrients without problematic amino acids. These specialized formulas can help patients meet nutritional requirements without worsening their condition.
Some patients may benefit from modified food preparations that reduce problematic amino acids. Examples include low-protein bread, pasta, and other staples that allow greater dietary variety.
Protein Distribution Guidelines:
- Spread protein intake throughout the day
- Focus on high-quality protein sources
- Adjust intake based on activity level and growth needs
Targeted Supplementation Strategies
Supplementation forms the cornerstone of treatment for many amino acid deficiencies. Essential amino acids that cannot be synthesized by the body must be supplied through diet or supplements.
For specific disorders, amino acid supplementation targets exactly what the body lacks. Doctors prescribe precise formulations based on blood tests and clinical presentation.
Single amino acid supplements help address specific deficiencies. For example, L-carnitine supplementation benefits several metabolic disorders by supporting fatty acid metabolism.
Common Therapeutic Supplements:
- Branched-chain amino acids (BCAAs)
- Essential amino acid mixtures
- Condition-specific amino acid formulations
- Vitamin cofactors (B6, B12, folate)
The timing of supplement intake matters significantly. Many practitioners recommend taking amino acid supplements between meals for better absorption and utilization.
Ongoing Monitoring and Support
Regular blood tests are essential to track amino acid levels and ensure treatments are working effectively. The frequency depends on the specific disorder and its severity.
Nutritional counseling provides patients with practical strategies for maintaining their specialized diets. Registered dietitians with expertise in metabolic disorders play a vital role in treatment teams.
Growth and development monitoring is crucial, especially for children with amino acid disorders. Regular height, weight, and developmental assessments help ensure the dietary restrictions aren't limiting proper growth.
Psychological support addresses the challenges of living with dietary restrictions. Support groups connect patients and families facing similar challenges and provide emotional resources.
Clinical Trials in Amino Acid Disorders
Therapeutic research continues to advance treatment options for amino acid disorders. Current clinical trials explore enzyme replacement therapies that could reduce dietary restrictions.
Gene therapy represents a promising frontier, potentially correcting the underlying genetic causes of amino acid metabolism disorders. Several trials are investigating gene delivery methods for various conditions.
Novel drug developments target specific metabolic pathways affected in amino acid disorders. These medications aim to improve quality of life by reducing the strictness of dietary management.
Participation in clinical trials offers patients access to cutting-edge treatments while contributing to scientific knowledge. Eligibility criteria vary by study, and patients should discuss options with their healthcare providers.
Researchers continue investigating dietary interventions like methionine restriction, which has shown promising results in extending lifespan in animal studies.
Managing Amino Acid Deficiency in Special Populations
Special medical conditions often require customized approaches to amino acid management. Certain genetic disorders affect how the body processes proteins and amino acids, requiring careful dietary planning and medical supervision.
Spinal Muscular Atrophy and Amino Acid Needs
Spinal Muscular Atrophy (SMA) is a genetic disorder that affects muscle strength and movement. Patients with SMA often experience muscle wasting which can impact protein metabolism and amino acid requirements.
Research indicates that people with SMA may benefit from specific branched-chain amino acid supplementation to help preserve muscle mass. Leucine is particularly important as it stimulates protein synthesis.
Dietary management for SMA patients typically includes:
- Higher protein intake (carefully balanced)
- Supplementation with essential amino acids
- Regular nutritional assessments
Medical supervision is crucial when implementing amino acid therapy for SMA patients. Dosages must be individualized based on disease severity, weight, and overall nutritional status.
Considerations in Cystic Fibrosis and CF
Cystic Fibrosis (CF) creates unique challenges for amino acid metabolism due to malabsorption issues and increased energy expenditure. CF patients often have higher protein needs than the general population.
Pancreatic insufficiency in CF patients can lead to poor protein digestion and subsequent amino acid deficiencies. Common signs include muscle weakness, poor growth, and delayed wound healing.
Treatment approaches include:
- Enzyme replacement therapy to improve protein digestion
- Higher protein intake (120-150% of standard requirements)
- Targeted amino acid supplementation
Regular monitoring of plasma amino acid levels helps guide treatment. Essential amino acids like arginine and glutamine may require special attention in CF patients due to their role in respiratory function and immune health.
Congenital Disorders: X-ALD, SCID, CAH
Several congenital disorders directly impact amino acid metabolism and require specialized management approaches.
X-linked Adrenoleukodystrophy (X-ALD) affects the breakdown of very long-chain fatty acids but can also influence amino acid processing. Dietary management focuses on balancing protein intake while restricting specific fats.
Severe Combined Immunodeficiency (SCID) patients often exhibit amino acid abnormalities that can worsen immune function. Careful supplementation of arginine and glutamine may support immune cell development.
Congenital Adrenal Hyperplasia (CAH) affects hormone production but also influences amino acid metabolism. Key considerations include:
- Monitoring for amino acid imbalances
- Adjusting protein intake during stress periods
- Supplementing with specific amino acids as needed
All these conditions require specialized care from metabolic specialists and regular assessment of amino acid status.
Specific Amino Acids: Functions and Deficiency Risks
The human body requires specific amino acids for various metabolic functions, and deficiencies in these critical building blocks can lead to distinctive health problems. Each essential amino acid plays unique roles in maintaining bodily functions, from neurotransmitter production to muscle development.
Phenylalanine and PKU
Phenylalanine is an essential amino acid that helps form neurotransmitters like dopamine and norepinephrine. These chemicals regulate mood, attention, and memory. The body converts phenylalanine into tyrosine, another important amino acid.
People with Phenylketonuria (PKU) cannot properly metabolize phenylalanine due to a genetic enzyme deficiency. This condition causes phenylalanine to build up to toxic levels, potentially leading to:
- Severe intellectual disability (if untreated in infancy)
- Seizures
- Behavioral problems
- Skin rashes
- Musty body odor
PKU requires strict dietary management, limiting foods high in phenylalanine such as meat, dairy, and artificial sweeteners containing aspartame. Early detection through newborn screening has dramatically improved outcomes for individuals with PKU.
Branched-Chain Amino Acids: Leucine, Isoleucine, Valine
Leucine, isoleucine, and valine are collectively called branched-chain amino acids (BCAAs) due to their molecular structure. These amino acids comprise about 35% of essential amino acids in muscle proteins and 40% of the body's total amino acid requirement.
BCAAs serve critical functions:
Leucine: Primarily stimulates protein synthesis and muscle growth
Isoleucine: Regulates energy and blood sugar
Valine: Supports muscle metabolism and tissue repair
Deficiencies in BCAAs may cause:
- Muscle wasting
- Poor wound healing
- Compromised immune function
- Fatigue and decreased endurance
Athletes and physically active individuals often supplement with BCAAs to improve recovery and reduce muscle breakdown during intense exercise.
Lysine, Biotinidase Deficiency, and Others
Lysine plays essential roles in calcium absorption, collagen formation, and immune function. This amino acid is particularly important for growth and tissue repair.
Lysine deficiency may manifest as:
- Anemia
- Reproductive disorders
- Hair loss
- Poor concentration
- Increased susceptibility to infections
Biotinidase deficiency, while not an amino acid deficiency itself, affects protein metabolism. This genetic disorder prevents the body from recycling biotin, a B vitamin crucial for amino acid processing.
Signs of biotinidase deficiency include:
- Seizures
- Skin rashes
- Hearing loss
- Developmental delays
Early diagnosis and treatment with biotin supplements can prevent these complications. The condition underscores how enzymatic processes affecting amino acid metabolism can create cascading health effects even when dietary intake is adequate.
Long-Term Outlook and Preventive Strategies for Amino Acid Deficiency
Managing amino acid deficiency requires a comprehensive approach that combines early detection with proper treatment strategies. Proper management can prevent serious health complications and improve quality of life for those affected.
Importance of Early Detection
Early detection of amino acid deficiencies is crucial for effective treatment and preventing long-term health problems. Diagnostic testing helps identify specific amino acid imbalances before symptoms become severe.
Blood tests, urine analysis, and genetic screening are the primary methods used to detect amino acid disorders. These tests measure amino acid levels and can identify metabolic abnormalities.
Some disorders, like phenylketonuria (PKU), are included in newborn screening programs in many countries. This early identification allows for immediate dietary intervention.
For adults experiencing symptoms, comprehensive amino acid panels can detect deficiencies that may be causing issues like muscle weakness, fatigue, or cognitive problems. The sooner treatment begins, the better the outcome typically is.
Preventing Cognitive Decline and Associated Complications
Amino acid deficiencies can lead to serious cognitive decline if left untreated. The brain requires specific amino acids to function properly and produce essential neurotransmitters.
Preventive strategies include:
- Regular monitoring of amino acid levels for those with known disorders
- Dietary management with proper protein intake
- Supplementation when medically necessary
- Medication adherence for specific amino acid disorders
For conditions like maple syrup urine disease or homocystinuria, strict dietary control is essential to prevent intellectual disability and neurological damage. These conditions require lifelong management.
Physical therapy and occupational therapy may help address complications that have already developed. Cognitive rehabilitation can also benefit those experiencing cognitive symptoms.
Family and Genetic Counseling
Many amino acid disorders result from genetic mutations that are inherited. Genetic counseling provides valuable information for families affected by these conditions.
Counselors help explain:
- The inheritance pattern of specific disorders
- Recurrence risks for future pregnancies
- Options for prenatal testing
- Available treatments and management strategies
For parents of affected children, understanding the genetic basis helps with family planning decisions. Carrier testing can identify individuals who carry a gene mutation but don't show symptoms.
Preconception genetic testing is recommended for couples with family histories of amino acid disorders. This allows for informed reproductive choices and early intervention when needed.
Support groups connect families with similar experiences, providing emotional support and practical advice for managing these complex conditions.
Additional Rare Disorders and Related Conditions
Beyond common amino acid deficiencies, several rare genetic disorders affect amino acid metabolism and can cause serious health complications. These conditions often present in early childhood and require specialized treatment approaches.
Isovaleric Acidemia and Glutaric Acidemia Type I
Isovaleric acidemia is a rare genetic disorder affecting the breakdown of the amino acid leucine. Symptoms typically appear during infancy and include:
- Strong, unpleasant body odor (described as “sweaty feet”)
- Poor feeding and vomiting
- Lethargy and seizures
- Developmental delays
Treatment focuses on a low-protein diet with special medical formulas that limit leucine intake. Supplementation with glycine and carnitine helps remove toxic metabolites from the body.
Glutaric acidemia type I results from the body's inability to process certain amino acids properly. It causes:
- Macrocephaly (enlarged head) at birth
- Progressive movement disorders, especially dystonia
- Sudden neurological crises during illness
Management includes a low-lysine diet, carnitine supplements, and emergency protocols during illness to prevent metabolic crisis.
Homocystinuria and Multiple Carboxylase Deficiency
Homocystinuria is characterized by elevated homocysteine levels in the blood and urine. This condition affects connective tissues, eyes, and the vascular system, causing:
- Tall, slender build with long limbs
- Lens dislocation in the eyes
- High risk of blood clots
- Skeletal abnormalities
Treatment typically includes vitamin B6 supplementation, which helps approximately 50% of patients. Others benefit from betaine, vitamin B12, and folate supplements along with a methionine-restricted diet.
Multiple carboxylase deficiency affects several critical metabolic pathways and presents with:
- Skin rash and hair loss
- Breathing problems
- Seizures and developmental delays
- Metabolic acidosis
Biotin supplementation effectively treats most cases, with dramatic improvement often seen within days of starting therapy.
Other Relevant Metabolic Diseases
Galactosemia is a disorder where the body cannot properly metabolize galactose, a sugar in milk. Though not directly an amino acid disorder, it shares similar metabolic pathways and management approaches. Symptoms include:
- Feeding problems and failure to thrive
- Jaundice
- Liver damage
- Cataracts
The primary treatment is the elimination of galactose and lactose from the diet, especially removing milk and dairy products.
Hartnup disease affects the transport of neutral amino acids, particularly tryptophan. Patients may experience:
- Pellagra-like skin rash with sun exposure
- Cerebellar ataxia (coordination problems)
- Psychiatric symptoms
Treatment includes niacin supplementation and a high-protein diet. Most patients respond well and can lead normal lives with proper management.
Citations and Scientific Sources
Proper scientific backing is crucial when discussing amino acid deficiency. The following resources provide reliable information for both researchers and individuals seeking evidence-based knowledge about amino acid disorders and treatments.
Utilizing PubMed and Scholarly Literature
PubMed offers extensive research on amino acid disorders, providing detailed information about how these compounds function as building blocks for cell repair and growth. This database contains thousands of peer-reviewed studies on amino acid metabolism.
Scientific journals such as Nature publish cutting-edge research linking amino acid metabolism disorders to various conditions including metabolic diseases, cardiovascular issues, and immune dysfunction.
ScienceDirect provides comprehensive overviews of amino acid deficiencies, noting that general signs often resemble those of kwashiorkor. Their articles specifically highlight how arginine deficiency can result in disease.
The National Center for Biotechnology Information offers valuable resources explaining how both animal and plant proteins contain approximately 20 common amino acids in varying proportions.
Frequently Asked Questions
Amino acid deficiency presents with specific symptoms that vary by severity, age, and gender. These conditions can affect multiple body systems and typically require targeted nutritional interventions for recovery.
What are the common symptoms of amino acid deficiency in adults?
Adults with amino acid deficiency often experience muscle loss as the body breaks down muscle tissue to access needed amino acids. This leads to weakness and reduced strength.
Physical signs include brittle or thinning hair, dry and flaky skin, and deep ridges on fingernails. These occur because protein is essential for maintaining these tissues.
Edema (swelling) may develop, particularly in the extremities, as protein helps maintain fluid balance in tissues. Increased hunger and frequent infections are also common due to compromised immune function.
What neurological impacts can result from protein deficiency?
Protein deficiency can cause increased anxiety and depression because amino acids are precursors to neurotransmitters that regulate mood. Without adequate amino acids, mood regulation becomes impaired.
Cognitive function may decline, resulting in poor concentration, memory issues, and mental fatigue. This occurs because proteins are needed for brain cell maintenance and neurotransmitter production.
Sleep disturbances are common, with sleep disorders often developing as amino acids help regulate sleep hormones and cycles.
What diseases are specifically linked to inadequate amino acid intake?
Kwashiorkor is a severe protein deficiency disease most commonly seen in developing regions. It causes edema, distended abdomen, and skin changes.
Arginine deficiency can result in specific diseases affecting multiple body systems. This essential amino acid is crucial for immune function and wound healing.
Muscle wasting disorders may develop with chronic protein deficiency. These conditions can become serious if left untreated and may lead to severe weakness and mobility issues.
What are the signs that a female might be experiencing protein deficiency?
Females with protein deficiency often experience hormonal imbalances affecting menstrual cycles. These disruptions occur because proteins are needed for hormone production.
Hair loss is particularly noticeable in females with amino acid deficiency. Women may notice thinning hair or increased shedding during brushing or washing.
Nail brittleness and slow growth are common signs. Women may observe that their nails break easily and don't grow as quickly as normal.
How can amino acid deficiency be effectively treated?
Dietary modifications are the primary treatment approach. Increasing high-quality protein sources like lean meats, eggs, dairy, legumes, and complete plant protein combinations is essential.
Amino acid supplements may be recommended in severe cases. These can target specific deficiencies when blood tests identify particular amino acids that are low.
Medical supervision is important during recovery, especially for severe deficiencies. A healthcare provider can monitor progress and adjust treatment as needed.
What is the typical recovery time for someone suffering from protein deficiency?
Mild deficiencies typically show improvement within 2-4 weeks of appropriate dietary changes. Energy levels and skin condition are often the first to improve.
Moderate to severe deficiencies may require 3-6 months for full recovery. The body needs time to rebuild tissues and restore normal function.
Recovery timeline varies based on deficiency severity, individual metabolism, age, and adherence to treatment plans. Consistent protein intake is necessary to maintain improvements and prevent relapse.
Conclusion
Recognizing the warning signs of amino acid deficiency early can prevent serious health complications. From muscle weakness to mood changes, these signals should never be ignored.
Proper diagnosis through blood tests and symptom evaluation is essential. Working with healthcare providers ensures accurate identification of specific amino acid imbalances.
Treatment approaches vary based on individual needs. Dietary adjustments often form the foundation of recovery, focusing on protein-rich foods like lean meats, eggs, dairy, and plant proteins.
Supplements may be necessary when diet alone isn't enough. These should always be taken under medical supervision to avoid new imbalances.
Lifestyle modifications complement other treatments. Regular exercise, stress management, and adequate sleep all support amino acid metabolism.
Prevention remains the best strategy. A balanced diet, regular health screenings, and awareness of your body's signals can help maintain optimal amino acid levels.
Remember that personalized care is crucial. What works for one person may not work for another, making professional guidance invaluable throughout the treatment process.
With proper attention and care, most amino acid deficiencies can be effectively managed, allowing for restoration of health and prevention of future issues.