Endometriosis is a health condition where tissue similar to the lining of the uterus grows in places outside the uterus. This tissue growth can lead to pain, irregular periods, and sometimes even problems with fertility. Endometriosis is most common in people between the ages of 15 and 44, but it can affect anyone with a uterus.
Some people may not even realize they have it, while others may experience severe symptoms that disrupt daily life. Learning more about endometriosis can help manage symptoms and improve quality of life. For more details about what endometriosis is and who it affects, visit the Mayo Clinic’s page on endometriosis.
Key Takeaways
- Endometriosis happens when tissue like the uterine lining grows outside the uterus.
- It can cause pain, period problems, and affect fertility.
- Treatment options are available to help manage symptoms and improve life quality.
Understanding Endometriosis
Endometriosis is a common yet often misunderstood health condition that affects a significant number of women and girls during their reproductive years. It involves the growth of tissue similar to the endometrium outside the uterus, causing inflammation, pain, and sometimes other complications.
What Is Endometriosis
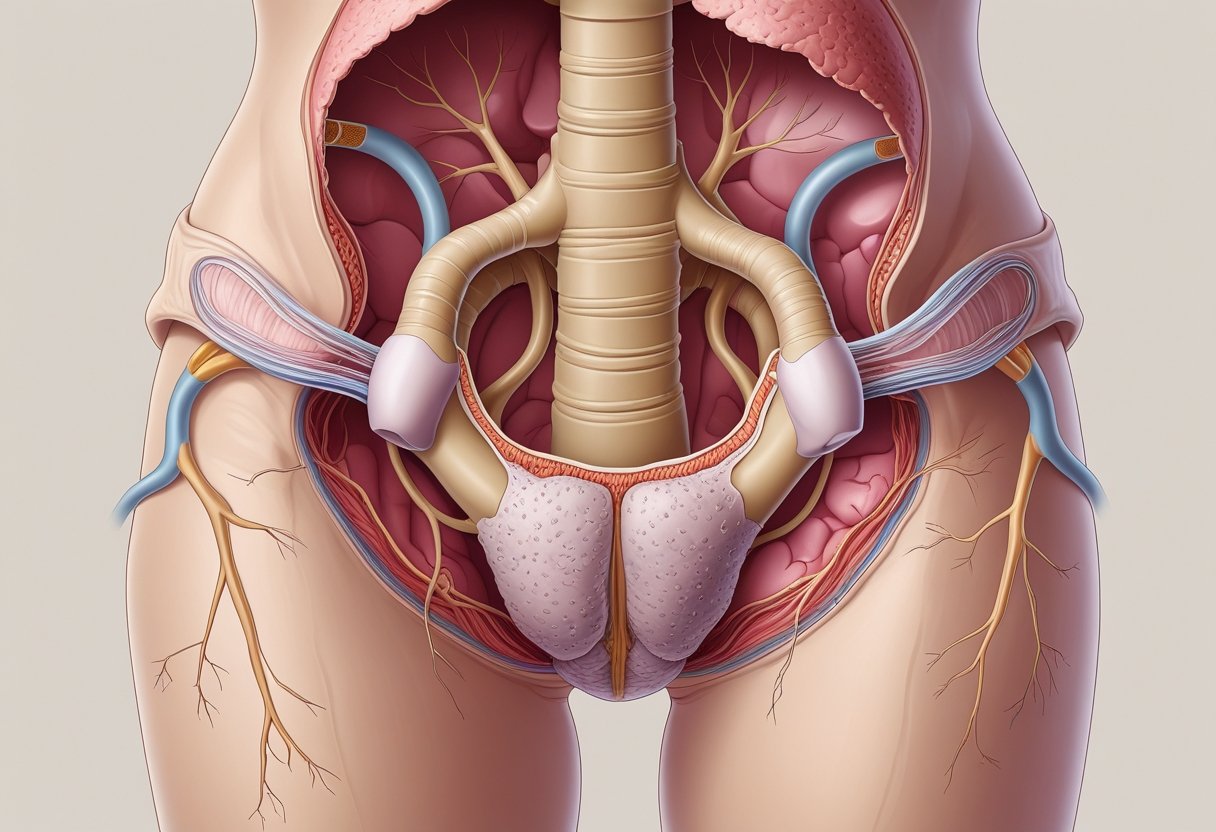
Endometriosis is a chronic and inflammatory condition where tissue that resembles the lining inside the uterus, called the endometrium, starts to grow outside the uterus. This tissue can develop on the ovaries, fallopian tubes, and other pelvic organs.
The misplaced tissue still acts like endometrial tissue: it thickens, breaks down, and bleeds with each menstrual cycle. However, because it has no way to exit the body, it can lead to irritation, scar formation, and sometimes problems with fertility. Women with endometriosis often have pelvic pain, especially during periods.
It is unrelated to cancer and is not an infection, but it does cause discomfort and can worsen over time if not managed. Endometriosis may lead to infertility in some cases.
Endometrial Tissue Growth
The tissue found outside the uterus in endometriosis is similar to, but not exactly the same as, the uterine lining. This abnormal growth usually occurs in the pelvic area but can sometimes be found in the abdomen or, rarely, in other parts of the body.
Common places for endometrial tissue growth:
- Ovaries
- Fallopian tubes
- Outer surface of the uterus
- Pelvic lining
As this tissue is hormone-responsive, it reacts to menstrual cycle changes. Each month, swelling, bleeding, and inflammation may occur, which can lead to chronic pelvic pain and the development of scar tissue or adhesions. Over time, these changes may cause organs to stick together or become damaged, potentially resulting in significant pain or organ dysfunction.
Prevalence and Impact
Endometriosis affects up to 10% of women and girls who are of reproductive age. While rare in girls who have not started puberty and women after menopause, it is most commonly found in those aged between 15 and 49.
The impact of endometriosis can be substantial. Many experience ongoing pain, heavy periods, and sometimes infertility. Symptoms often lead to missed work or school, emotional distress, and reduced quality of life.
A timely and accurate diagnosis can be challenging because symptoms often mimic other problems. Delayed diagnosis is common, making awareness and early medical attention important for managing this inflammatory condition.
Symptoms and Signs
Endometriosis is linked to different symptoms that affect the body in specific ways. The most noticeable issues are pain symptoms, changes in the menstrual cycle, and discomfort in the pelvic area.
Pain Symptoms
People with endometriosis often report different types of pain. The pain can happen before or during periods and even when periods are not occurring. Many experience pain in the lower back, lower abdomen, or pelvic region.
Pain during intercourse is another symptom that some notice. This pain might be deep and can affect daily activities and relationships. Some people also have pain while using the bathroom or during urination and bowel movements, especially around the menstrual period.
Pain can range from mild to severe. The severity is not always linked to the amount of tissue growth. Even small areas of endometriosis can cause intense pain in some people. For more about these symptoms, the NHS has an overview.
Menstrual Cramps and Dysmenorrhea
Menstrual cramps, also called dysmenorrhea, are a common sign of endometriosis. These cramps often start before the period begins and can be worse than regular period pain.
Women may notice cramps in the lower abdomen or pelvic area. The pain may even spread to the lower back or down the legs. It can last several days and may not improve much with common pain medicines.
Some people may notice that the cramps are worse over time or last longer than usual. Severe cramps can make it hard to go to work or school or do daily activities.
A detailed list of these symptoms can be found from Pinnacle Fertility.
Abdominal Bloating and Heavy Periods
Endometriosis can also cause abdominal bloating. This feeling of fullness or swelling is sometimes called “endo belly.” The stomach may look or feel larger than usual, and clothes may fit tighter during this time.
Heavy periods, known as menorrhagia, are also linked to endometriosis. Periods might last longer or cause someone to change pads or tampons more often than normal. There may be blood clots or spotting between periods.
People may feel tired or weak if there is too much blood loss. The heavier-than-usual periods can interrupt daily routines and lower energy levels. For more information on these signs, visit the Cleveland Clinic's endometriosis page.
Chronic Pelvic Pain
Chronic pelvic pain means long-lasting pain in the lower abdomen or pelvis. With endometriosis, this pain may not be tied to the menstrual cycle and can be present every day.
The pain can feel dull or sharp. It might come and go, or be constant. Some people say it gets worse with certain activities like standing, walking, or after physical exercise.
This kind of pain can make it hard to sleep, stay active, or keep up with friends and work. Doctors may ask about this when making a diagnosis, as chronic pelvic pain is a key symptom of endometriosis. More specifics about pelvic pain can be found at Johns Hopkins Medicine’s resource.
Causes and Risk Factors
Endometriosis develops when tissue that looks like the lining of the uterus grows outside of it. Key risk factors include genetics, menstrual cycle patterns, and lifestyle choices such as physical activity and body mass index.
Genetic and Environmental Factors
A person is more likely to get endometriosis if someone in their family, such as a mother or sister, has the condition. This shows that genes play a strong role in passing on the risk. Studies have found that women with a family member affected by endometriosis have a higher chance of being diagnosed themselves.
Environmental factors also matter. Exposure to some chemicals in the environment, like dioxins and some pesticides, may increase risk. These chemicals can affect how the body deals with hormones and may disturb the normal function of the reproductive system. Both genetics and environmental exposures can make symptoms worse or make them start earlier for some people. For more detailed information on these risks, visit What are the risk factors for endometriosis?.
Role of Menstrual Cycle
Menstrual cycle patterns are strongly linked to endometriosis risk. Those who started their periods at a younger age or have short cycles (less than 27 days) are more likely to develop the condition. Long and heavy periods also add to the risk.
Conditions that block or slow the flow of menstrual blood, such as a closed hymen or uterine abnormalities, can make it more likely for tissue to travel where it shouldn’t. Not giving birth and not breastfeeding are linked with a higher chance of being diagnosed as well. Find more about these links in the section about endometriosis risk factors from Johns Hopkins Medicine.
Body Mass Index and Physical Activity
Body weight and physical activity levels may also affect the risk. People with a lower body mass index (BMI) are sometimes found to have a slightly higher risk of developing endometriosis, though the reason is not fully clear. On the other hand, regular exercise may help lower risk by improving hormone balance and reducing inflammation.
Staying active can help regulate menstrual cycles and support a healthy weight. While exercise is not a guarantee for prevention, a balanced lifestyle may lower the chance of developing symptoms. For more on lifestyle and risk, read the Cleveland Clinic's guidance on endometriosis.
Diagnosis of Endometriosis
Endometriosis can be challenging to confirm, and it often requires several steps. Doctors use a combination of symptom review, physical exams, imaging, and sometimes surgery to reach a diagnosis.
Clinical Evaluation and History
A careful clinical evaluation begins with a detailed medical history. Doctors ask about symptoms such as pelvic pain, menstrual cramps, irregular periods, and pain during sex or bowel movements. These symptoms are often the first clues.
Questions about the timing, frequency, and severity of pain help doctors understand its pattern. They also review any previous treatments, family history of endometriosis, and current medications.
A thorough history is important because endometriosis can have symptoms similar to other conditions. By carefully listening to the patient’s experience, doctors can decide which tests are most useful. A good history can increase the sensitivity of further diagnostic steps by pointing to likely causes.
Pelvic Examination
During a pelvic examination, the doctor checks for tenderness, nodules, or masses in the pelvic area. This exam is done while the patient is lying down, and the doctor may palpate with their fingers to feel for abnormalities.
The exam may be uncomfortable, but it can give important information. Sometimes, doctors feel small lumps or areas of thickening behind the uterus or along the pelvic wall.
While a pelvic exam alone cannot confirm endometriosis, it can reveal signs that suggest the condition. The sensitivity of this exam depends on how advanced the endometriosis is and where the tissue is located.
Imaging Techniques
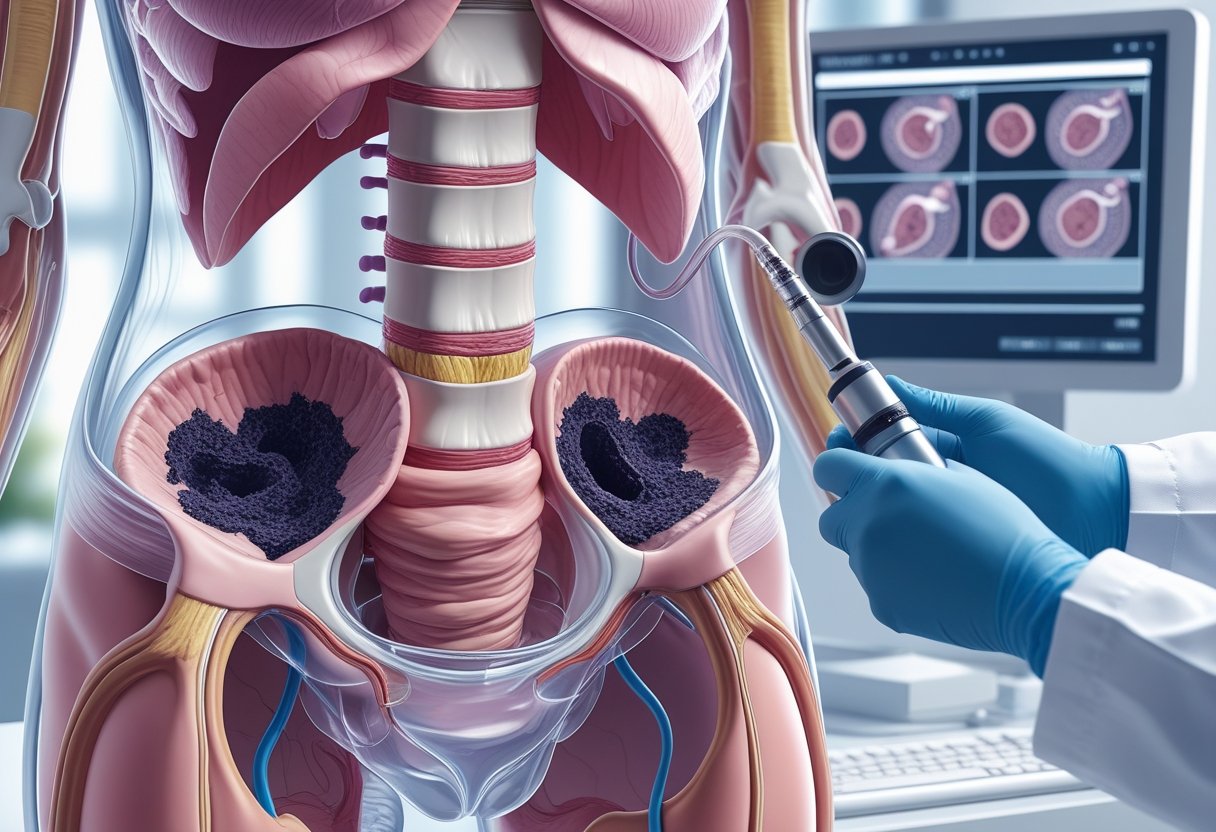
Imaging methods, like transvaginal ultrasonography and magnetic resonance imaging (MRI), are used to look for signs of endometriosis inside the pelvis.
Transvaginal ultrasonography involves a small probe placed inside the vagina, which creates images of the uterus, ovaries, and pelvic area. This test can detect large ovarian cysts (endometriomas) linked to endometriosis.
Magnetic resonance imaging (MRI) uses strong magnets and radio waves to produce detailed images. MRI can help show the size and location of endometriosis tissue more clearly than ultrasound, especially in more complicated cases.
Both techniques have limits. They do not always find smaller spots of endometriosis, so they are mostly used when deeper or cystic disease is suspected.
Definitive Diagnosis Methods
The only way to confirm endometriosis is through surgery. The most common type is laparoscopy, a minimally invasive procedure where a small camera is inserted into the abdomen.
During laparoscopy, the doctor looks for endometriosis tissue directly. If suspicious areas are seen, a biopsy (a small tissue sample) can be taken and checked by a lab. This is important for histologic confirmation and ensures an accurate diagnosis.
Laparoscopy allows for both diagnosis and sometimes treatment in the same procedure. According to major medical organizations, this remains the standard for the definitive diagnosis of endometriosis. However, doctors may rely on symptoms and noninvasive tests before recommending surgery.
Complications and Associated Conditions
Endometriosis can cause several health issues besides pain. It may affect fertility, create growths in and around the ovaries, and lead to tissue sticking together inside the pelvis.
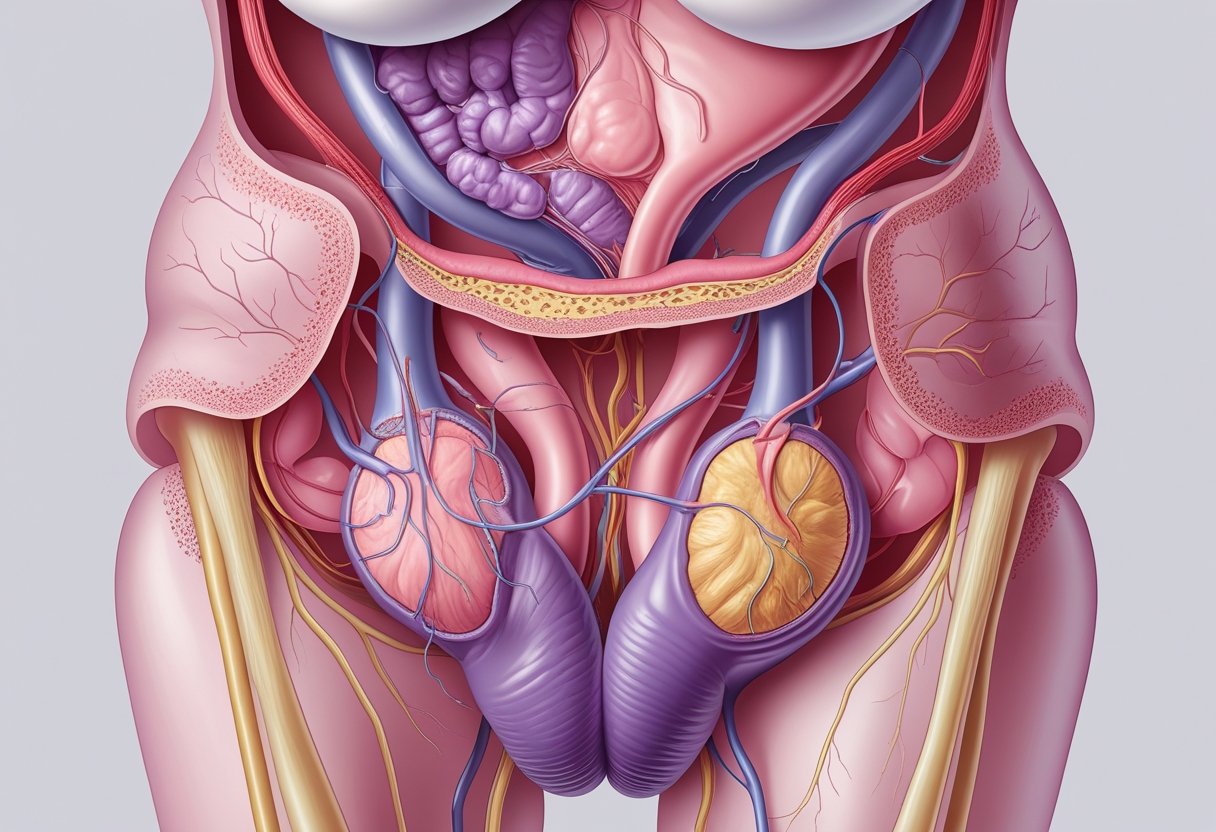
Infertility and Fertility Challenges
Around 30% to 50% of people with endometriosis have problems getting pregnant. The patches of tissue can harm the ovaries, fallopian tubes, or uterus, making it harder for eggs and sperm to meet. In some cases, the reason for being unable to conceive is called unexplained infertility.
The inflammation and scarring caused by endometriosis can block the fallopian tubes. Even without a clear blockage, the condition can damage egg quality or change how the uterus works. Treatments like surgery or IVF may help some people have children.
Ovarian Cysts and Endometrioma
Endometriosis can lead to the formation of ovarian cysts, also called endometriomas. These cysts are sometimes called “chocolate cysts” because they contain dark, old blood. They can cause pelvic pain, especially during menstrual periods, and may be found during routine ultrasounds.
Endometriomas can impact the normal tissue of the ovaries and lower the number of healthy eggs. Large cysts may need to be removed if they cause pain or grow in size. In some cases, repeated surgeries for cysts can lower ovarian reserve, making fertility management more complicated. Read more about ovarian cysts and endometrioma.
Adhesions and Pelvic Inflammation
Endometriosis often creates scar tissue, called adhesions, which can cause organs to stick together. Adhesions make pelvic pain worse and may affect how organs work. Sometimes, these tissues connect the uterus, bowels, bladder, or ovaries in ways that can cause long-term pain and bowel or urinary problems.
Pelvic inflammation is another problem. The constant irritation can lead to swelling and more scar tissue in the area. In severe cases, adhesions may need to be surgically removed to ease pain or improve organ function. More information on adhesions and pelvic inflammation is available online.
Treatment Options for Endometriosis
Treatment for endometriosis depends on the severity of symptoms, age, and whether pregnancy is desired. Some people find relief with medications, while others may need a mix of approaches or even surgery.
Pain Relief and Pain Medications
Pain management is one of the first steps for people dealing with endometriosis. Over-the-counter pain medicines such as acetaminophen can be helpful for mild cramps or pelvic pain. Doctors may also prescribe stronger painkillers for those with severe pain symptoms.
Prescription medications can target pain directly. Sometimes, nerve pain medicines are used if regular painkillers are not effective. These strategies do not treat the cause but help people be more comfortable.
Physical therapy and lifestyle changes may also play a role. Many patients combine pain medication with approaches like warm baths and regular exercise. For details on treatment plans, Johns Hopkins Medicine discusses pain management for endometriosis.
Hormonal Therapies
Hormonal therapy helps slow the growth of endometrial tissue outside the uterus. Hormonal contraceptives like birth control pills, patches, and vaginal rings work by controlling periods and lessening pain. They can be helpful for people who do not want to get pregnant right away.
Other options include gonadotropin-releasing hormone (GnRH) agonists and antagonists. These drugs put the body into a temporary menopause-like state, lowering estrogen and shrinking endometrial growths. Side effects can include hot flashes or bone thinning.
Additional choices are danazol and aromatase inhibitors. Danazol lowers the body’s estrogen but is less commonly used due to side effects. Aromatase inhibitors block estrogen production and are sometimes given with other drugs.
Hormonal IUDs (intrauterine devices) are another option. They release progestin to decrease pain and reduce bleeding. Details on these therapies are available from Mayo Clinic’s endometriosis treatment section.
Nonsteroidal Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to treat pain and inflammation in endometriosis. Examples include ibuprofen and naproxen. These drugs block chemicals that cause inflammation in the body.
NSAIDs are usually the first treatment tried for menstrual cramps and mild pelvic pain. They are easy to get and are safe for short-term use. Taking NSAIDs before the start of a period may help reduce pain levels.
These medicines do not stop endometriosis from growing but are useful for many people. Combination with other treatments, like hormonal therapy, may offer better relief. For more on the use of NSAIDs and other medicine options, see information from the Cleveland Clinic treatments for endometriosis page.
Surgical Management
Surgery for endometriosis often focuses on removing or destroying abnormal tissue to help reduce pain and improve quality of life. Careful planning and technique can help lower risks and support healing.
Laparoscopic Surgery
Laparoscopic surgery is the standard way to treat endometriosis. This method uses small cuts and a camera to see inside the body. The surgeon removes or burns away endometriosis tissue while trying to avoid healthy organs.
This type of surgery is less invasive than open surgery. It leads to shorter hospital stays, less pain, and a quicker return to normal activities. Surgeons can remove cysts, scar tissue, and implants while leaving the uterus and ovaries when possible.
Laparoscopic procedures are also used to confirm the diagnosis of endometriosis. The technique allows for both diagnosis and treatment at the same time. For more details, the NYU Langone Health article on surgical treatment for endometriosis provides a useful overview.
Surgical Treatment Outcomes
The results of surgery depend on the stage and location of the disease. Pain relief is common, especially in the first year after surgery. Surgery may also improve fertility for some women with mild or moderate endometriosis.
Sometimes, the disease can return, especially if all tissue is not removed. Repeat surgery is possible but can carry increased risks like scar tissue or damage to organs. Other treatments, such as hormones, may be recommended after surgery to help prevent a recurrence.
Patients should talk with their doctor about risks and benefits. Laparoscopic surgery is preferred over open surgery for most people. More information about outcomes is available in the Cleveland Clinic’s guide to endometriosis surgery.
Managing Postoperative Pain
After surgery, pain is managed using a mix of medicines and self-care steps. Doctors often suggest over-the-counter pain relievers at first. Sometimes stronger medication is needed if pain is severe. Ice packs, rest, and gentle movement can help with healing.
Doctors may recommend pelvic floor therapy or light activity to help prevent stiffness. Monitoring for signs of infection or unusual pain is important. Some people may need additional help for ongoing or severe pain, as recovery can vary.
Patients should follow their care plan and let their provider know if pain does not improve. Early support can make recovery smoother and help prevent long-term discomfort. The Mayo Clinic’s endometriosis treatment overview offers more details about managing symptoms after surgery.
Advanced and Adjunctive Therapies
Some people with endometriosis need more than standard treatments. Others may seek advanced options when pain or infertility continues despite trying medication or minor procedures.
In Vitro Fertilization and Assisted Reproduction
For people struggling to conceive, in vitro fertilization (IVF) is a common next step. IVF involves retrieving eggs, fertilizing them in a lab, and transferring healthy embryos to the uterus. This helps bypass blockages or damage caused by endometriosis.
Success rates for IVF can depend on age, egg quality, and the extent of endometriosis. Patients with severe cases may need extra steps, such as surgical removal of endometrial tissue or hormone treatments before IVF cycles.
Other assisted reproductive technologies (ART) may include intrauterine insemination (IUI) or using donor eggs. These options can be discussed with a fertility specialist, and choices depend on patient needs and medical history.
Clinical Trials and Experimental Treatments
Researchers are developing new ways to manage pain and target endometriosis at its source. Some promising developments include immunotherapy, gene therapy, and targeted medications that impact hormones or inflammation. Many of these treatments are still being tested in ongoing clinical trials and experimental studies.
Patients can join clinical trials to access cutting-edge medicines, such as GnRH antagonists or treatments using regenerative medicine. Others explore new options like photodynamic therapy and stem cell therapies, although these are not yet part of routine care. Participation criteria vary, so patients should discuss eligibility, risks, and benefits with their medical team.
Living With Endometriosis
People living with endometriosis often deal with pain, fatigue, and changes in their daily routines. Managing the condition involves understanding its impact and finding ways to support physical and emotional health.
Quality of Life Considerations
Endometriosis can cause chronic pelvic pain, painful periods, and pain during sex. Some people experience discomfort so severe it disrupts work, school, and daily activities. Symptoms also include heavy bleeding and digestive issues like bloating or constipation.
The emotional effects should not be overlooked. Ongoing pain may lead to stress, anxiety, or depression. Relationships and intimacy may become strained by the physical and emotional challenges. Studies show that endometriosis may even impact sexual desire and emotional wellbeing.
Difficulty getting pregnant is another concern. Some people with endometriosis face issues with fertility, which can add to emotional distress. Seeking care from a healthcare provider familiar with endometriosis is important for addressing both physical and mental wellbeing.
Coping Strategies and Support
Several coping strategies can help manage life with endometriosis. Regular exercise has been shown to relieve pain by increasing blood flow and triggering endorphin release, which are the body’s natural painkillers. Even light activities like walking or stretching can be helpful.
A balanced, healthy diet may ease digestive problems and help the body handle inflammation. Tracking symptoms in a journal helps some people recognize patterns and triggers for their pain. Many benefit from joining a support group, which offers a safe space to share experiences and tips with others who understand the condition. For more specific guidance, resources about living with endometriosis provide advice on self-care and emotional support.
Seeking help from mental health professionals, when needed, is also important. Therapy and counseling offer tools for managing stress, anxiety, and depression related to the condition.
Frequently Asked Questions
Endometriosis is a progressive condition that can cause pain, fertility issues, and other symptoms. Understanding the causes, treatments, and impacts on health helps people manage the condition more effectively.
What treatment options are available for endometriosis?
Treatment options include medication, hormone therapy, and surgery. Pain relievers and anti-inflammatory drugs can reduce discomfort. Hormonal treatments may slow the growth of endometrial tissue. In some cases, doctors suggest surgery to remove endometrial tissue if other treatments do not help.
What are the common symptoms associated with endometriosis?
Common symptoms are painful periods, heavy menstrual bleeding, and pain during sex. Some people experience pain during urination or bowel movements. Others may notice fatigue, digestive problems, or trouble getting pregnant. For more details, review information on symptoms of endometriosis.
Can endometriosis be effectively managed with surgery?
Surgery can remove patches of endometrial tissue. Some people feel relief after surgery, but symptoms sometimes return over time. Surgery is an option if other treatments do not control pain or if fertility is a concern. Surgical techniques may include laparoscopy or, in severe cases, hysterectomy.
What factors contribute to the development of endometriosis?
The exact causes are unclear, but genetics may play a role. Menstrual flow that travels backward into the pelvis and problems with immune response are possible factors. Family history of endometriosis increases risk. Environmental factors have also been suggested but are still being studied. More details can be found from endometriosis frequently asked questions.
How can one receive a definitive diagnosis for endometriosis?
Diagnosis usually starts with a medical history and physical exam. Imaging tests like ultrasound may help, but laparoscopy is the only way to confirm endometriosis. During laparoscopy, a doctor looks inside the abdomen and may take a tissue sample for testing. Learn more about diagnosing endometriosis.
What is the impact of endometriosis on fertility and pregnancy?
Endometriosis can make it harder to get pregnant. Some people may need fertility treatments. Even with endometriosis, many people do get pregnant. If pregnancy is a goal, early treatment and advice from a doctor can help increase the chances. More information about fertility and pregnancy in endometriosis is available.
Conclusion
Endometriosis affects millions of women and adolescents. It involves tissue similar to the lining of the uterus growing outside the uterus, which can cause pain and impact daily life. Early recognition of symptoms is important for better care.
Common symptoms of endometriosis include:
- Pelvic pain
- Painful periods
- Heavy menstrual bleeding
- Pain during intercourse
- Infertility
Diagnosis often takes time, as symptoms can be confused with other conditions. Delays can lead to ongoing discomfort and frustration. Healthcare providers use physical exams, imaging tests, and sometimes surgery to confirm endometriosis.
Multiple treatment options exist. These include pain medicines, hormone therapy, and surgery. The choice depends on the patient's age, symptoms, and desire for future pregnancy. Guidelines from leading organizations can help guide management. Details about the clinical management of endometriosis are explained by specialists.
Key concerns for people with endometriosis:
| Concern | Description |
|---|---|
| Quality of life | Daily activities can be limited |
| Emotional health | Chronic pain may lead to stress or sadness |
| Fertility impact | Some have trouble getting pregnant |
Awareness, open discussions, and access to care support people living with endometriosis. New research, better guidelines, and early management can help improve outcomes. More information on endometriosis care can be found from health organizations like the World Health Organization.

